Managing Male Sexual Problems Related to Cancer
Sex, sexuality, and intimacy are just as important for people with cancer as they are for people who don’t have cancer. In fact, sexuality and intimacy have been shown to help people face cancer by helping them deal with feelings of distress, and when going through treatment. But, the reality is that a person's sex organs, sexual desire (sex drive or libido), sexual function, well-being, and body image can be affected by having cancer and cancer treatment. How a person shows sexuality can also be affected. Read more in How Cancer and Cancer Treatment Can Affect Sexuality and Cancer, Sex, and the Male Body.
Managing sexual problems is important, but might involve several different therapies, treatments, or devices, or a combination of them. Counseling can also be helpful. The information below describes ways to approach some of the more common sexual problems an adult male with cancer may experience. If you are a transgender person, please talk to your cancer care team about any needs that are not addressed here.
Communication about sexuality is key
It’s very important to talk about what to expect, and continue to talk about what's changing or has changed in your sexual life as you go through procedures, treatments, and follow-up care. Don't assume your doctor or nurse will ask you about any concerns you have about sexuality. Remember, if they don't know you're having a problem, they can't help you manage it. Here are some ways you can start talks with your cancer care team about the problems you might be having.
Know when to ask questions
The best time to talk with your doctor or cancer team about possible side effects or long-term changes in your sex life is when making treatment decisions or before treatment. If this isn't possible, or you don't think about asking these kinds of questions before surgery or treatment, you can start to talk with them shortly after surgery or when treatment starts. But you can bring up the subject any time during and after treatment, too.
Ask the right questions
It’s important to know what to expect. When you are asking questions before treatment, here are some that can open the door to more questions and follow-up:
- Will my treatment (surgery, radiation, chemo, hormone therapy, etc) affect my sex life? If so, what can I expect?
- Will the effects last a short time, a long time, or be permanent?
- What can be done about these effects? Is there a cost to what can be done?
- Can I see a specialist or counselor?
- Are there any other treatments that are just as effective for my cancer but have different side effects?
- Do you have any materials I can read or can you suggest where I can find more information?
Maybe you've already had surgery or started treatment, but didn't ask questions (or get enough information) beforehand. Maybe you've read some things on the internet or heard about someone else's experience with the same type of cancer you have. Maybe you're able to think more clearly now than when you were first diagnosed and realize you have questions. Whatever the reason, if you wondering about something, ask! Here are some ways to start talking with your cancer care team:
- "I was reading about (surgery/treatment) and that it might cause sexual problems. Can you explain that to me?"
- "I know someone who went through this same thing and heard about problems they had with sex. Can you give me more information about this?"
- "I am having trouble adjusting to some changes in my body. What can I do?"
Learn as much as possible
Once you have a discussion and keep talking, it's easier to get and find the information you need. Knowing answers to the questions you have, and knowing what to expect, can help you and your partner understand what's ahead. Be careful about where you get information. Ask your cancer care team to recommend where to find credible, current, accurate information. Sexual problems caused or worsened by anxiety can often be helped through counseling with a mental health therapist who specializes in dealing with sexual issues. If a treatment or therapy is recommended, learn as much about it as possible and be sure to check with your insurance company about coverage. You can call the American Cancer Society, too, and we can help guide you: 1-800-227-2345.
Include your partner
It's best to include your partner in any decision about therapies, treatments, or devices. Sexual sharing and emotional closeness are ways a couple can feel close during the stress of an illness. It's important for your partner to understand the procedure and have a chance to discuss any fears or questions with you and the health care team.
Managing common sexual problems in adult males with cancer
Erectile dysfunction (ED)
The success rates of treatments to help with erectile dysfunction (ED) vary greatly, and you may have to try a few to find the one that works best for you. In many cases, sexual counseling can help a couple discuss their options and plan how to make the new treatment a comfortable part of their sex life. Sometimes penile rehabilitation is an option. This involves the use of ED medications along with other therapies. Learn more in How Cancer Can Affect Erections.
Pills
Drugs for ED come in pill form. All of these drugs help a man get and keep an erection by causing more blood to flow into the penis. If you are having trouble with erections, these pills are often the first type of treatment recommended. However, certain operations (such as a prostatectomy) can affect the nerves that help cause erections. These pills work with the nerves responsible for erections. And even with nerve-sparing surgery (saving the nerves responsible for erections that run close to the rectum and along the prostate), the nerves might still be damaged and need time to heal (sometimes up to 2 years). Many men may find the pills don’t work well during the first few months after surgery, but they might be more helpful as time goes by. At 18 to 24 months after surgery, the pills may be helpful in getting a firm erection.
Be sure your doctor knows about all medicines you take, even supplements, over-the-counter medicines, and vitamins, because some can interact with ED drugs or other treatments. Make sure you understand all side effects of ED pills that are prescribed for you, and that you know when to get help for any of them. You should only take these pills if they are prescribed by your doctor and come from a legitimate pharmacy. Avoid buying medicines that claim to treat ED but don't need a prescription. There’s a large counterfeit market for pills for ED. These pills are usually not effective for helping erections and may be dangerous.
Penile injections
Another option is to inject the penis with a medicine that causes erections. A very thin needle is used to put the drug into the side of the shaft of the penis a few minutes before starting sexual activity. The combination of sexual excitement and medicine helps to produce a firmer and longer-lasting erection. Penile injections are the most reliable treatment for ED, and work in many men who try them. The first injection is usually done in the doctor’s office, where the doctor can teach the man how to do the next ones at home. Although they are effective much of the time, many men feel nervous and anxious about having a penile injection and giving it themselves. If penile injections are an option you're thinking about, be sure to know and understand both short-term and long-term side effects.
Urethral pellets
Another way to help with erections is a urethral pellet, or medicated urethral system for erection (MUSE). An applicator is used to put a tiny pellet (called a suppository) of medicine into his urethra (the opening at the tip of the penis). As the pellet melts, the drug is absorbed through the lining of the urethra and enters the spongy tissue of the penis. The man must urinate before putting in the pellet so that the urethral lining is moist. After the pellet is put in, the penis must be massaged to help absorb the medicine. This system may be easier than injections, but it doesn’t always work as well. Be sure you understand all possible side effects if you're thinking about using a MUSE.
Vacuum erection devices
To help with ED or penile shortening, a vacuum erection devices (VEDs) work well for some men. With a VED, the man places a plastic cylinder over his penis and pumps out air to create a vacuum around the outside of the penis. The suction draws blood into the penis, filling up the spongy tissue. When the penis is firm, the man takes the pump off and slips a stretchy band onto the base of his penis to help it stay erect. The band can be left on the penis for up to half an hour.
Some men use the pump before starting sexual touching, but others find it works better after some foreplay has produced a partial erection. It may take some practice to learn how to use a VED and be comfortable using it. Most vacuum devices are prescribed by doctors, but some are available over the counter.
Penile implants (prostheses)
For men who have tried all the treatments listed above and have not found one that works well, surgery to implant a prosthesis in the penis may be an option to consider. Over the past several decades, many of these operations have worked well to treat permanent erection problems. Most men who have implant surgery are pleased with the results.
There are different types of implants. Which one may be best depends on the age, body size, penile size, history, needs, and preferences of the man who is thinking about it as an option. An inflatable implant can have either 2 or 3 pieces.
- For a 3-piece implant, an inflatable cylinder is put inside the penis, and a balloon-shaped reservoir (storage tank) that contains fluid is tucked behind the groin muscles. The fluid usually stays in the reservoir, leaving the cylinders in the penis empty. A pump is placed inside the loose skin of the scrotal sac. All the parts are connected with tubing. Squeezing the pump moves the fluid from the reservoir into the cylinder, creating an erection. When the pump is released, the fluid goes back into the reservoir, emptying the penis again.
- For a 2-piece inflatable implant, most of the fluid is in the back of the cylinders, and the pump is put into the scrotum.
A semi-rigid or non-inflatable implant is a less common type of prosthesis that uses semi-rigid rods that are implanted in the penis. When a man wants an erection, he bends the rods up; otherwise he bends them down. This is a simpler device to use than an inflatable implant, but is less like a normal erection.
Learn as much as you can and ask your urologist questions about the pros and cons of each type of implant before making your decision.
Testosterone therapy
If a man has a hormone imbalance, testosterone may restore his desire and erections. Having low testosterone can lead to low sexual desire and trouble with erections. It can also lead to a loss of energy. If you think you might have low testosterone, it’s important to talk to your cancer care team. Tests can be done to find out your testosterone level, and you can discuss possible treatment options. However, testosterone is not right for everyone, even if they have low testosterone levels, and is usually not given to men who have had certain types of cancer.
Herbs or natural remedies
Many herbal and dietary supplements are sold over the counter claiming to be “natural” cures for erection problems. These supplements have not been proven to help men regain erections. It’s important to know that supplements are not strictly regulated in the United States like drugs are. Supplement makers don’t have to prove their products are effective (or even safe) before selling them. Some supplements might not even contain the ingredients on their labels, while others might contain other (potentially harmful) ingredients.
Be sure to talk to your doctor about any supplement or other over-the-counter treatment you are thinking about trying.
Dry, painful, or weak orgasms
Some men treated for cancer don't have fluid come out of their penis when they ejaculate because of surgery that has removed the seminal vesicles. This is called having a dry orgasm. While it can take a while to adjust to having dry orgasms after surgery, they don't need treatment. Men who have dry orgasms after cancer treatment also say they sometimes have reduced sensation.
Some men might notice that their orgasms become weaker or last a shorter time than before. As men age, the muscle contractions at climax are no longer as strong. But, more severe weakening of orgasm often goes along with erection problems. In these cases, treating the erection problem may not improve a man’s orgasm. Orgasms are possible without an erection or full erection. A sex therapist can give you guidance and instruction on techniques that can help stimulate an erection.
Painful orgasm may also be a side effect of surgery. If this happens, medication to manage the pain or seeing a sex therapist may be helpful.
Special aspects of some cancers and cancer treatments
Urostomy, colostomy, or ileostomy
An ostomy allows waste to leave the body through a surgical opening (stoma) in the skin and into a pouch that you can empty.
- A urostomy takes urine through a new passage and sends it out through an opening on the belly (abdomen).
- Colostomy and ileostomy are both openings on the abdomen for getting rid of fecal waste (stool) from the intestines. In an ileostomy, the opening is made with the part of the small intestine called the ileum. A colostomy is made with a part of large intestine called the colon.
There are ways to reduce the effect an ostomy has on your sex life. First, make sure your appliance (pouch system) fits well. Check the seal, and empty your ostomy bag before sex. This will reduce the chance of a leak. Learn more in Ostomies.
Tracheostomy and laryngectomy
A tracheostomy is a surgery that removes the windpipe (trachea). It can be temporary or permanent, and you breathe through a stoma (opening or hole) in your neck.
Laryngectomy is surgery that removes the voice box (larynx). It leaves you unable to talk the usual way, and since the larynx is next to the windpipe that connects the mouth to the lungs, you breathe through a stoma (opening or hole) in your neck.
A scarf, ascot tie, or turtleneck can look good and hide the stoma cover. During sex, a partner may at first be startled by breath that hits at a strange spot, and this might take some getting used to. You might also have food odors coming from the stoma. You can lessen odors from the stoma by avoiding garlic or spicy foods and by wearing cologne or after-shave lotion.
Sometimes problems speaking can make it hard for couples to communicate during sex. If you have learned to speak using your esophagus, talking during sex is not a big problem. A speech aid or electronic voice box also work well.
Treatment for head and neck cancer
Some cancers of the head and neck are treated by removing part of the bone structure of the face. This can change your appearance. Surgery on the jaw, palate, or tongue can also change the way you look and talk. Facial reconstruction can help regain a more normal look and clearer speech.
Limb amputation
Treatment for some cancers can include surgically removing (amputating) a limb, such as an arm or leg. A patient who has lost an arm or leg may wonder whether to wear his artificial limb (prosthesis) during sex. Sometimes the prosthesis can help with positioning and ease of movement.
Loss of a testicle
Treatment for testicular cancer usually means removal of one or both testicles, or testes (orchiectomy). Although some men are not upset about the loss of a testicle, others may fear a partner’s reaction. Since this operation also removes the epididymis above the testicle, that side of the scrotum looks and feels empty. To get a more natural look, a man can have a testicular prosthesis put in his scrotum during surgery. The prosthesis can be sized to match the remaining testicle.
Penile shrinkage after prostatectomy
After prostate surgery, a penis may be shorter than before, much like what happens in cold water. Penile shrinkage is common after surgery. The cause of penile shrinkage might have to do with surgery affecting the nerves that control erection. Blood flow changes, scarring, and changes in penile tissue that result from loss of erections also may play a role. There’s no known way to prevent or treat penile shrinkage at this time. Some studies suggest early penile rehabilitation can help decrease shortening, and vacuum devices might be helpful.
Cancer of the penis
When a man has cancer of the penis or of the bottom end of the urethra, the treatment may be to remove part or all of the penis (penectomy). These operations can have a major effect on a man’s self-image and his sex life. Penile-sparing techniques are used as often as possible. These include local treatments and limited surgeries, to save as much of the penis as possible to preserve sexual function, the way the penis looks, and the ability to urinate while standing up. Examples are a circumcision, simple excision, Mohs surgery. And, if the procedure is a partial penectomy, the glans or head might be removed. In these cases, a man can still reach orgasm and have normal ejaculation.
A total penectomy removes the entire penis, including the base that extends into the pelvis. The surgeon creates a new way for urine to leave the body through an opening between the man’s scrotum and his anus (the outside opening of the rectum). The man can still control his urination because the “on-off” valve in the urethra is above the level of the penis.
Feeling good about yourself and feeling good about sex
Sometimes friends and lovers do withdraw emotionally from a person with cancer. Don’t give up on each other. It may take time and effort, but keep in mind that sexual touching between a man and his partner is always possible. It may be easy to forget this, especially if you’re both feeling down or have not had sex for a while. Review Cancer, Sex, and the Male Body for some tips to help you and your partner through this time. And keep in mind that you may need extra help with the changes caused by cancer that can turn your and your partner’s lives upside down.
Overcoming anxiety about sex
Sometimes because of a cancer-related symptom or treatment side effect, it might not be possible to be as spontaneous as you were in the past. The most important thing is to open up the topic for discussion and begin scheduling some relaxed time together.
Masturbation is not a required step in resuming your sex life, but it might help. It can also help you find out where you might be tender or sore, so that you can let your partner know what to avoid.
Sexual activity with your partner
Just as you learned to enjoy sex when you started having sex, you can learn how to feel pleasure during and after cancer treatment.
Depending on your situation, you may feel a little shy. It might be hard to let your partner know you would like physical closeness, so be as clear and direct as you can.
Don’t give up, and keep talking to your partner.
Making sex more comfortable
If you still have some pain or feel weak from cancer treatment, you might want to try new sex positions. Talk to your partner and learn different ways to enjoy sex that are most comfortable. The drawings below are some ideas for positions that may help in resuming sex.
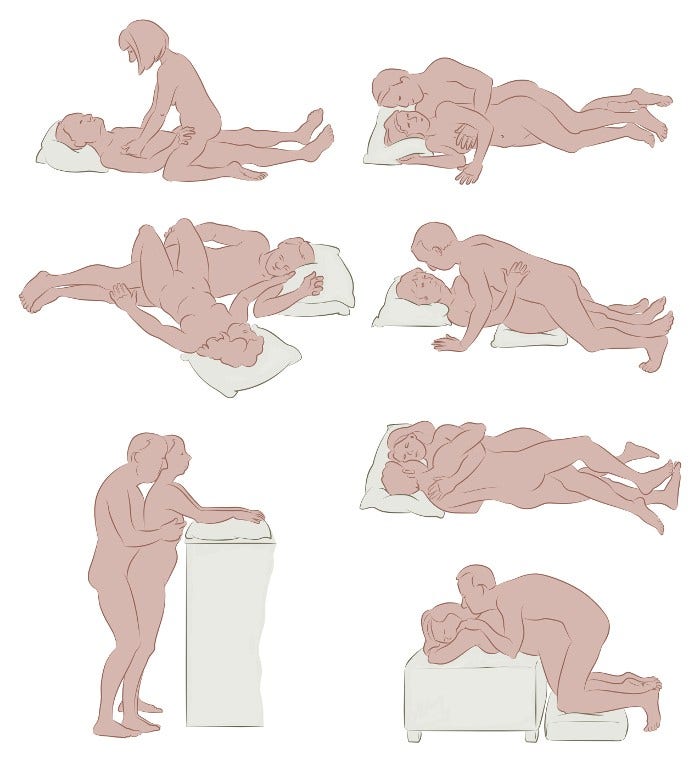
There’s no one position that’s right for everyone. You and your partner can work together to find what’s best for you. Pillows can help as supports. Keeping a sense of humor can always lighten up your efforts.
- Written by
- References

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
American Association of Clinical Endocrinologists. American Association of Clinical Endocrinologists Medical Guidelines for Clinical Practice for the Evaluation and Treatment of Male Sexual Dysfunction: A couple’s problem – 2003. Update Endocr Pract. 2003;9(No. 1). Accessed at https://www.aace.com/sites/default/files/2019-06/sexdysguid.pdf on January 31, 2020.
Carter et al. Interventions to address sexual problems in people with cancer: American Society of Clinical Oncology clinical practice guideline adaptation of Cancer Care Ontario guideline. Journal of Clinical Oncology. 2018;36(5):492-513.
Katz A. Breaking the Silence on Cancer and Sexuality: A Handbook for Healthcare Providers. 2nd ed. Pittsburgh, PA: Oncology Nursing Society.; 2018.
Katz, A. Man Cancer Sex. Pittsburgh: Hygeia Media, 2010.
Khera M, Snyder PJ, Martin KA. Treatment of male sexual dysfunction. UpToDate. 2019. Accessed at https://www.uptodate.com/contents/treatment-of-male-sexual-dysfunction on January 31, 2020.
Moment A. Sexuality, intimacy, and cancer. In Abrahm JL, ed. A Physician’s Guide to Pain and Symptom Management in Cancer Patients. Baltimore, MD: Johns Hopkins University Press; 2014:390-426.
National Comprehensive Cancer Network (NCCN). Clinical practice guidelines in oncology: Survivorship [Version 2.2019]. Accessed at https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf on January 31, 2020.
Nishimoto PW, Mark DD. Sexuality and reproductive issues. In Brown CG, ed. A Guide to Oncology Symptom Management. 2nd ed. Pittsburgh, PA: Oncology Nursing Society; 2015:551-597.
Schover LR. Sexual healing in patients with prostate cancer on hormone therapy. ASCO Education Book. 2015;e562-566.
Zhou ES, Bober SL. Sexual problems. In DeVita VT, Lawrence TS, Rosenberg SA, eds. DeVita, Hellman, and Rosenberg’s Cancer: Principles and Practice of Oncology. 11th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2019:2220-2229.
Last Revised: February 5, 2020
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.


