ACS Research News
Published on: January 22, 2026
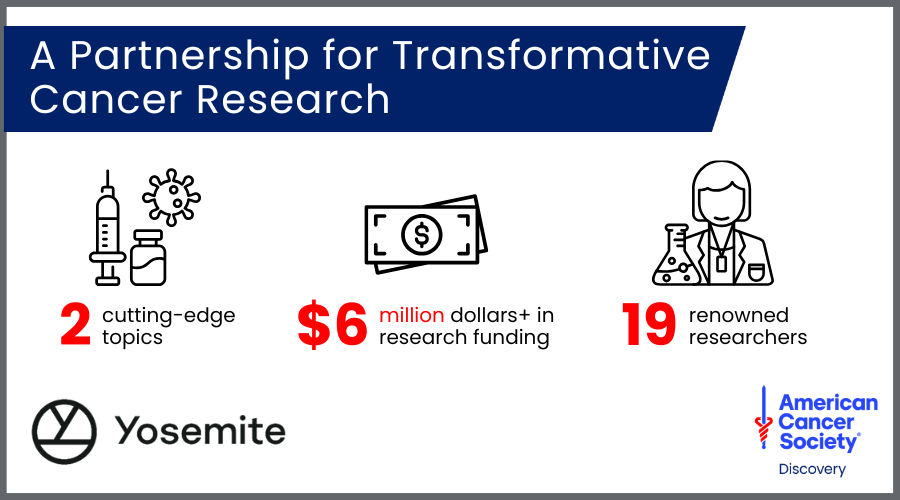
Awardees will receive $330,000 grants co-funded by Yosemite and the American Cancer Society to pursue critical cancer research.
Published on: January 13, 2026
Milestone in cancer survival: 7 in 10 people reach the 5-year mark
Published on: December 4, 2025
The updated guideline for cervical cancer screening introduces the option of self-collection of vaginal samples for HPV testing and new guidance on when screening can end.
Published on: September 12, 2025
The American Cancer Society awarded 14 new Discovery Boost grants and 4 new Mission Boost grants across 17 institutions this fall.