Your gift is 100% tax deductible.
Types of Tracheostomies
A tracheostomy is an opening in the front of the neck that’s made during an emergency procedure or a planned surgery. It makes an airway for people who are not breathing on their own, cannot breathe well, or have a blockage that is affecting their breathing. Sometimes people who have a disease, such as cancer, may need a tracheostomy if their disease is expected to soon cause breathing problems.
How long will I need my tracheostomy?
You may only need a tracheostomy for a short time (temporary). Or you may need a tracheostomy for the rest of your life (permanent).
- A temporary tracheostomy may be used if you have a blockage or injury to your windpipe. You might also need it if you need to be on a breathing machine (ventilator), such as for severe pneumonia, a major heart attack, or stroke.
- A permanent tracheostomy might be needed if part of your trachea needs to be removed because of a disease such as head and neck cancer.
If your tracheostomy is meant to be temporary, how long you need it depends on why it was placed and how long that problem will take to get better. For example:
- If you are given a tracheostomy because your doctor is worried about swelling from surgery or radiation therapy, you will need the tracheostomy until the swelling goes down.
- If you have trouble breathing on your own, you may need your tracheostomy until you no longer need a breathing machine.
- If you have a blockage, injury, or disease in your trachea, you will probably need a tracheostomy for a longer period of time.
How might my tracheostomy be placed?
How your tracheostomy is placed depends on why you need it. If you are having trouble breathing in an emergency, your tracheostomy may be placed where you are – usually in an emergency department or critical care unit so you can be watched closely. It can also be placed during a planned surgery to treat your cancer or other problems.
Like any procedure, getting a tracheostomy can cause side effects. You might has pain or discomfort, bleeding from your stoma, or infection.
A tracheostomy or laryngectomy tube will be placed once your tracheostomy is created. Nurses will take care of your tracheostomy and teach you how to care for it once you can go home.
Tracheostomy and laryngectomy tubes
Depending on how long you need your tracheostomy and the reason you had it placed, you will likely need to keep a tracheostomy or laryngectomy tube in the hole in your neck, at least for a while.
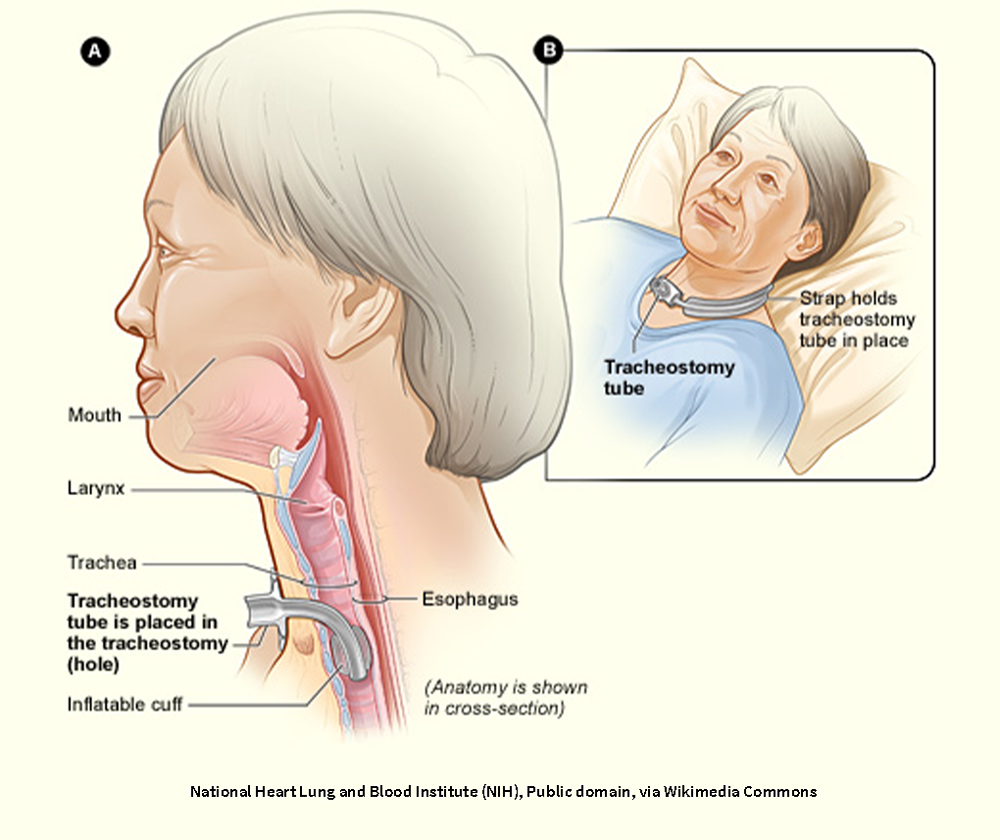
Tracheostomy tube
A tracheostomy tube is placed in your neck between your nose and your lungs. It helps make sure that you have a way to get air into your lungs when your airway is blocked, damaged, or swollen, or you need help breathing for more than a few days.
Tracheostomy tubes are either cuffed or uncuffed. The cuff is a seal that inflates inside your trachea to block air from leaking around the tube. It forces all air going in and out of the lungs to go through the tube and stops saliva and other liquids from getting into your lungs.
- A cuffed tube is often used when you need a ventilator (breathing machine) to help you breathe. The cuff pressure is monitored by your health care team and adjustments are made to the breathing machine as needed. A cuffed tube makes it hard for you to talk.
- Uncuffed tubes are used if you don’t need a ventilator. With an uncuffed tube, some air can still flow around the tube and up through your trachea to your larynx so you can talk.
Your tracheostomy may or may not have an inner cannula, depending on the type you have. An inner cannula is a liner that can be locked into place and then unlocked when you need to change or clean it.
Laryngectomy tubes and buttons
If you have had your larynx removed and don’t need help breathing, you might have a laryngectomy tube or button. These devices help keep your stoma open as you heal from surgery.
Laryngectomy tubes and buttons are softer, shorter, and wider than tracheostomy tubes and will adapt to the shape of your stoma. After your laryngectomy has healed, you might not need to use the laryngectomy tube or button. Talk to your doctor about whether you need to continue to use these devices once your stoma has healed.
- Written by
- References

Developed by the American Cancer Society medical and editorial content team with medical review and contribution by the American Society of Clinical Oncology (ASCO).
American Thoracic Society. Living with a tracheostomy. Accessed at https://craftprd1.blob.core.windows.net/documents/advocacy-patients/patient-resources/tracheostomy-in-adults-2.pdf on May 12, 2025.
Chee YMM, Roche E, Tay CAG. A Novel Improvised Laryngectomy Button Designed From A Milk Bottle Teat. OTO Open. 2023;7(4):e85. Published 2023 Nov 29. doi:10.1002/oto2.85
Hoffman MR. Tracheostomies and PEGs: When are they really indicated? Surg Clin North Amer. 2019;99(5):955-965.
Hyzy RC, McSparron JI. Tracheostomy: Postoperative care, maintenance, and complications in adults. UpToDate. 2025. Accessed at https://www.uptodate.com/contents/tracheostomy-postoperative-care-maintenance-and-complications-in-adults on May 16, 2025.
Hyzy RC, McSparron JI. Tracheostomy: Rationale, indications, and contraindications. UpToDate. 2024. Accessed at https://www.uptodate.com/contents/tracheostomy-rationale-indications-and-contraindications on May 12, 2025.
Ignatavicius DD, Rebar CR. Heimgartner NM. Medical-Surgical Nursing, 11th ed. Elsevier; 2024.
Last Revised: July 1, 2025
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.



