Your gift is 100% tax deductible.
Skin Cancer ACS Research Highlights
Skin cancer is by far the most commonly diagnosed cancer in the United States.
We know a lot about what causes skin cancer, and researchers are making more progress by using what we know to better understand the best ways to prevent and treat it.
Spotlight on ACS Research Publications
The American Cancer Society (ACS) employs a staff of full-time researchers and funds scientists across the US who relentlessly search for answers to help us better understand cancer, including skin cancer. Here are some highlights of their work.
ACS Cancer Prevention Studies
Studying Skin Cancer Causes and Prevention
The Cancer Prevention and Survivorship team in the American Cancer Society’s Population Science Department:
- Analyzes data about the link between lifestyle and skin cancer on an ongoing basis through the Cancer Prevention Study II (CPS-II). It began in 1982 and tracks about 1.2 million American men and women from all 50 states.
- Conducts Cancer Prevention Study 3 (CPS-3) to better understand ways to prevent cancer, including skin cancer. It started in 2013 and includes over 304,000 American men and women from all over the US and Puerto Rico.
Skin Cancer Cancer Facts & Figures in Brief
Facts About Skin Cancer
The American Cancer Society (ACS) publishes Cancer Facts & Figures each year. This report gives detailed analyses of how many people in the US develop and die from cancer. It includes the latest information on risk factors, early detection, treatment, and current research for the most common types of cancer.
Skin cancer is the most commonly diagnosed cancer in the US, with more than 5 million new cases diagnosed each year. Here are some other key facts about skin cancer for 2022:
Basal cell and squamous cancers are the most commonly diagnosed skin cancers in the US.
- Basal cell and squamous cell cancers are also called nonmelanoma skin cancer. It’s not unusual for a person to have more than one of these cancers on their skin at the same time. In fact, the most recent study estimated that in 2012 over 5 million cases of these cancers were diagnosed in more than 3 million people.
- Almost all cases of basal and squamous cell cancers skin cancer can be cured, especially if they are found and treated early.
Melanoma skin cancer death rates have dropped steeply because of advances in treatment.
- Melanoma accounts for only about 1% of skin cancers but causes a large majority of skin cancer deaths.
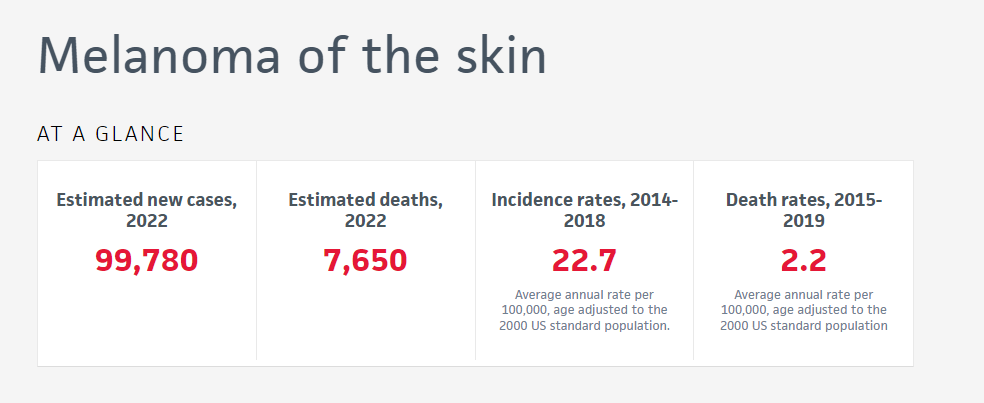
- About 99,780 Americans are expected to be diagnosed with melanoma in 2022. About 7,650 are expected to die from it.
- Melanoma mortality dropped steeply from 2015 to 2019 by about 4% per year because of the immunotherapy drug Yervoy (ipilimumab) and the targeted therapy drug Zelboraf (vemurafenib).

Find more statistics about melanoma on the Cancer Statistics Center:
- Estimated new cases and deaths
- Historical trends in incidence rates
- Historical trends in death rates
- 5-year survival rates
Use the analysis tool in the drop-down menu to see any of these statistics in comparison to other types of cancer.
More Skin Cancer Research Stories
We Fund Cancer Researchers Across the US
The American Cancer Society funds scientists who conduct research about cancer at medical schools, universities, research institutes, and hospitals throughout the United States. We use a rigorous and independent peer review process to select the most innovative research projects proposals to fund.
Stats on the left are as of February 20, 2025.