Your gift is 100% tax deductible.
Types of Urostomies
There are 2 main types of urostomies, often called urinary diversions. They are named for how they are created and whether urine output can be controlled or not.
Many factors must be considered when deciding which type of stoma you will need. Your surgeon will talk with you to help you decide which is your best option.
Incontinent urostomy
Incontinent diversions are the simplest type of urinary diversion. They do not have a way to keep urine inside of your body and drain often. You always need to keep a pouch on the outside of your body .
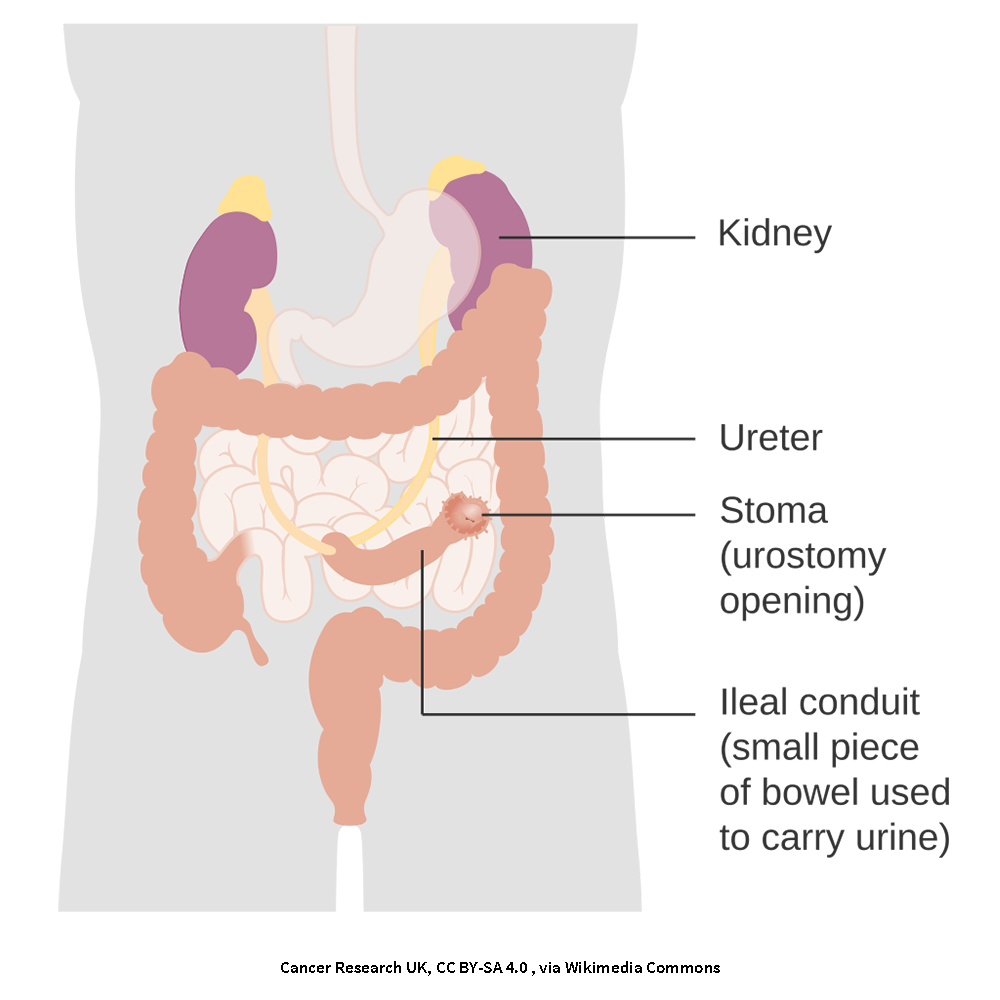
An ileal conduit is the most common type of incontinent diversion. It is made by creating a conduit (pipeline) from a piece of your small intestine.
A 10-to-15-centimeter (about 6- inch) piece of the lower part of the small intestine (called the ileum) is removed near where it attaches to the large intestine (colon). The rest of the ileum is then re-connected to the large intestine so that your bowels continue to work as they usually do.
Your ureters are detached from your bladder and attached to the piece of ileum. One end of the ileum is sewn closed to create a conduit for your urine to drain through. The other end of the piece of ileum is brought through the front of the abdomen to form the stoma.
After surgery, you may have thin tubes called stents coming out of your stoma. You may see the end of the tubes in your pouching system on the outside of your body to collect urine. The stents help protect the connections between your kidneys and the conduit. Your surgeon will remove the stents when they think you have healed enough.
An ileal conduit is permanent. Your urine will flow through the conduit and your stoma. You will always need to wear a collection pouch on the outside of your body.
You may also see mucus come through your stoma since your small intestine produces mucus naturally. This mucus will collect in the pouch along with the urine. This is normal.
Some incontinent diversions can also be made from part of your large intestine. They are less common but work the same way as an ileal conduit.
Continent urostomy
Continent diversion allows you to control when you urinate (pass urine). Some (such as an orthotopic urinary diversion or neobladder) let you urinate the same way you did before surgery.
With other continent diversions, you need to insert a catheter into a stoma to drain your urine. Continent urostomies can be created using different methods and might be called Indiana, Miami, or Kock pouches. But all require you to drain them several times a day.
The surgery to create a continent urostomy is similar to placing an incontinent diversion. However, your surgeon creates a pouch inside your body to hold the urine. The pouch has ‘valves’ to keep the urine in the pouch until you’re ready to empty it.
You empty this pouch several times a day by inserting a thin, flexible tube called a catheter into your urostomy stoma. The doctor or ostomy nurse will teach you how to drain the pouch and help you make a schedule to do it.
What should I expect when my urostomy is placed?
A urostomy is placed during surgery while you are under general anesthesia. Your urostomy may be placed during open surgery or laparoscopic surgery. Your surgeon can tell you which they think is best and why.
Like any other surgery, having a urostomy can have side effects. You will be at risk of bleeding or blood clots, urine leakage from your suture lines, infection, and damage to nearby organs. You may also notice changes in how your bowels work as you recover from surgery.
You will likely need to stay in the hospital for 5 to 10 days after your urostomy is placed. How long you stay will depend on why you need the urostomy and the type of urostomy you have. You will usually be able to go home once your urostomy is working and you are ready to care for it at home.
Complete recovery from an ileostomy may take 3 to 6 months. During this time, you might need to be careful about what you eat and drink.
- Written by
- References

Developed by the American Cancer Society medical and editorial content team with medical review and contribution by the American Society of Clinical Oncology (ASCO).
American Society of Clinical Oncology. Urostomy. Cancer.net. Content is no longer available.
Babakhanlou R, Larkin K, Hita AG, Stroh J, Yeung SC. Stoma-related complications and emergencies. Int J Emerg Med. 2022;15(1):17. Published 2022 May 9. doi:10.1186/s12245-022-00421-9
Barone B, Napolitano L, Reccia P, et al. Advances in Urinary Diversion: From Cutaneous Ureterostomy to Orthotopic Neobladder Reconstruction-A Comprehensive Review. J Pers Med. 2024;14(4):392. Published 2024 Apr 8. doi:10.3390/jpm14040392
Berti-Hearn L, Elliott B. Urostomy care: A guide for home care clinicians. Home Healthcare Now. 2019; 37(5):248-255.
Carmel J, Colwell JC, Goldberg M. Wound, Ostomy, and Continence Nurses Society Core Curriculum: Ostomy Management. 2nd ed. Wolters Kluwer Health; 2022.
Shariat SF, Bochner BH, Donahue TF, Pietzak EJ. Urinary diversion and reconstruction following cystectomy. UpToDate. 2024. Accessed at https://www.uptodate.com/contents/urinary-diversion-and-reconstruction-following-cystectomy on May 6, 2025.
United Ostomy Association of America (UOAA). Urostomy guide. Accessed at https://www.ostomy.org/wp-content/uploads/2018/03/UrostomyGuide.pdf on May 6, 2025.
Last Revised: July 1, 2025
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.



