Your gift is 100% tax deductible.
Cancer Disparities Research
We put cancer disparities research into action by providing evidence to inform cancer prevention and control initiatives that promote health equity.
What We Do
Cancer disparities are adverse differences between certain population groups across the cancer continuum, from prevention and screening through treatment and survivorship.
Cancer disparities may occur based on where people live, race/ethnicity, socioeconomic status (such as income or education level), sex, sexual identity or orientation, mental or physical ability, immigration status, and so on.
For example, from 2016 to 2020 colorectal cancer mortality rates were:
- 23% higher in nonmetropolitan areas than in large metropolitan areas
- 34% higher among Black populations than White populations
The American Cancer Society (ACS) Cancer Disparity Research team conducts transdisciplinary research to both:
- Identify individual, social, biological, structural, and system-level determinants of health
- Quantify the effect social determinants of health have on cancer disparities across the cancer continuum, including cause (etiology), prevention, screening and detection, incidence, stage at diagnosis, treatment, survivorship, quality of life after cancer treatment, and mortality
Our ultimate goal is to provide evidence to inform cancer prevention and control initiatives that promote health equity.
Glossary for Nonscientists
Featured Term: Social Determinants of Health
Social determinants of health are non-medical factors that influence health, the ability to function, risk for health problems, and quality of life. These include conditions in the environments where people are born, live, work, play, learn, worship, and age as well as the social, economic, and political systems that shape those conditions of daily life.
Social determinants of health are comprised of structural inequalities,* social injustices, and institutional environments.
The occurrence of cancer can be positively or negatively, affected by social determinants of health based on how they affect educational and job opportunities, income, housing, transportation, public safety, food security, social inclusion and non-discrimination, and access to affordable health services of high quality. Social determinants of health are closely linked with health disparities and cancer disparities.
*Bold terms are also in the glossary for nonscientists.
Factors Contributing to Cancer Disparities
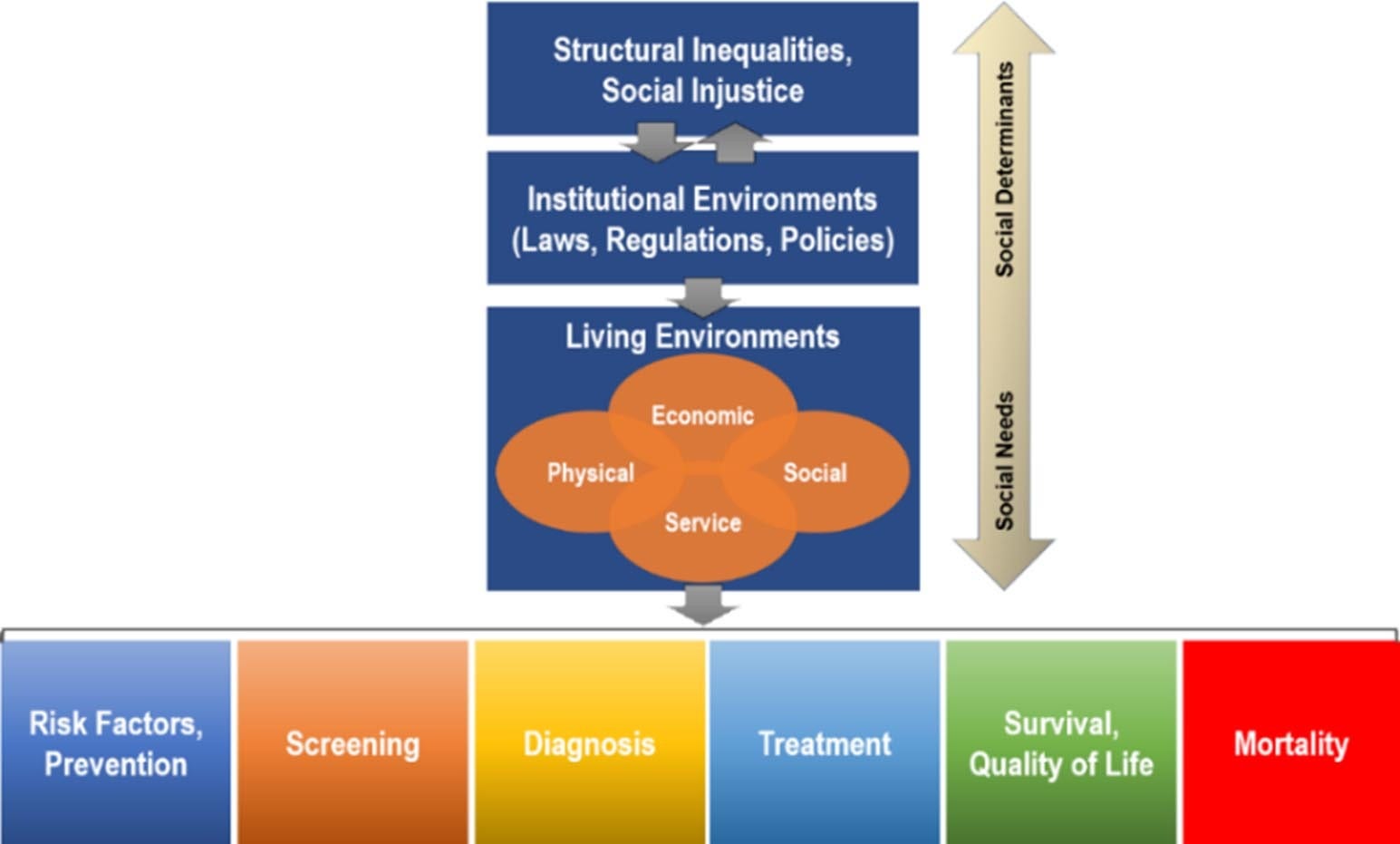
This graphic shows that:
- Social determinants of health are comprised of structural inequalities, social injustices, and institutional environments.
- Structural inequalities in an area (such as the number of hospitals or safe neighborhoods to play and exercise in) and social injustice (such as racism, homophobia, and gender inequality) influence and are influenced by institutional environments (laws, regulations, and policies that may affect civil and political rights).
- Laws, regulations, and policies affect conditions and opportunities where people live related to economics, social relationships, available services, and the physical environment.
- People’s living environments affect health outcomes across the cancer continuum, from prevention to mortality.
As part of our research, we seek to develop and use innovative methods to better disentangle the complex associations between social determinants of health and cancer disparities and provide evidence that can be used to mitigate these unjust differences.”

Our Work
The ACS Cancer Disparities Research Team
These cancer disparities researchers are part of the larger Surveillance, Prevention, & Health Services Research (SPHeRe) department:
Farhad Islami, MD, PhD, Senior Scientific Director
Daniel Wiese, PhD, Principal Scientist
Parichoy Pal Choudhury, PhD, Principal Scientist
Hyunjung Lee, PhD, Principal Scientist
Jordan Baeker Bispo, PhD, Principal Scientist
Dongjun Lee, MS, Associate Scientist II








