Your gift is 100% tax deductible.
Lung Cancer Research Highlights
Lung cancer is the leading cause of cancer death among both men and women
in the United States. Our research program has played a role in many of the prevention, screening, and treatment advances that save lives from lung cancer today. And, we continue to fund research to help save even more lives in the future.
Survival After a Diagnosis of Lung Cancer Has Improved, Yet More People Die from Lung Cancer Than Any Other Type
Over the past 20 years, there have been exciting improvements in survival after a diagnosis of lung cancer. In the mid1990s, 5-year relative survival was 15%, and between 2014 to 2020 it increased to 27%. These improvements may be related to:
- Diagnoses made at an earlier stage than they used to be, and earlier stages tend to be less complicated to treat.
- Advances in treatment such as targeted therapies.
Despite this progress, smoking is still responsible for most deaths from lung cancer.
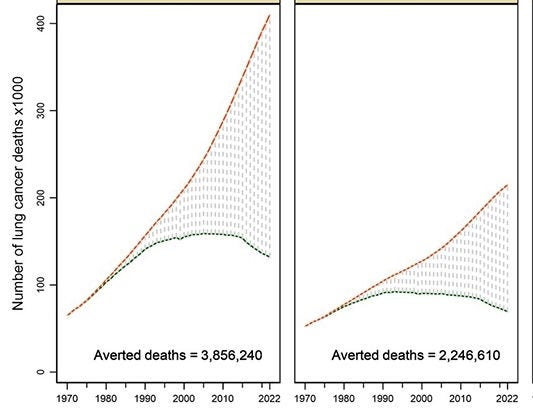
The Health Benefits of Stopping Smoking
Sources: Smoking Cessation. A Report of the Surgeon General Full Report, 2020 and The US Tobacco Atlas
Support for Quitting Smoking
- Map: Medicaid Coverage for Smoking Cessation
- Text Alternative
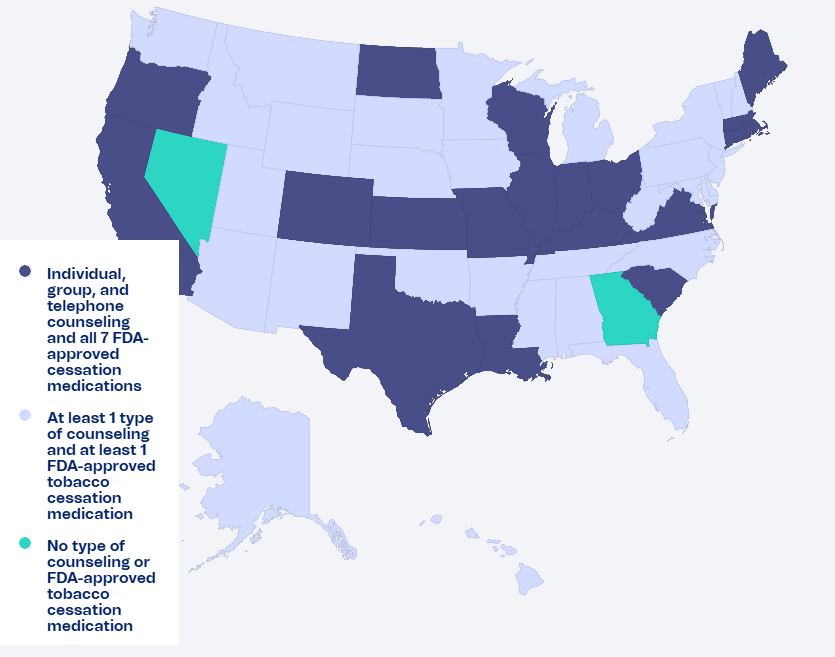
Source: The US Tobacco Atlas
Text Alternative for Map: Medicaid Smoking Cessation Coverage in the US, June 2024
Medicaid coverage for smoking cessation programs varies by state.
For these states, Medicaid covers counseling for individuals, groups, and by telephone, and all 7 FDA-approved smoking-cessation medications:
California
Colorado
Connecticut
Indiana
Illinois
Louisiana
Kansas
Kentucky
Maine
Massachusetts
Missouri
North Dakota
Ohio
Oregon
Rhode Island
Texas
Virginia
Wisconsin
South Carolina
For these states, Medicaid covers at least 1 type of counseling and at least 1 FDA-approved tobacco cessation medication:
Alabama
Alaska
Arizona
Arkansas
Delaware
Florida
Hawaii
Idaho
Iowa
Maryland
Michigan
Minnesota
Mississippi
Montana
Nebraska
New Hampshire
New Jersey
New Mexico
New York
North Carolina
Oklahoma
Pennsylvania
South Dakota
Tennessee
Utah
Vermont
Washington
West Virginia
Wyoming
For these states, Medicaid does not cover any type of counseling or FDA-approved tobacco cessation medication:
Georgia
Nevada
Our US Tobacco Atlas Provides an Interactive Platform to Bring Us Closer to a World Where No One Has Cancer Because of Tobacco
The ACS US Tobacco Atlas provides a state-by-state snapshot of where we stand and what we can do to close gaps in tobacco control. The Atlas provides compelling visuals and evidence that we can use in research, advocacy, public health, and community engagement.

Risk & Prevention Studies
Screening & Early Detection Studies
Ever Smoked Heavily? If So, You May Be Eligible for Lung Cancer Screening
Your primary care or specialty care providers are directed by the 2023 lung cancer screening guideline to refer you for screening with low-dose computed tomography (LDCT) every year if all of the following statements are true:
- You are between 50 and 80.
- You currently smoke or used to smoke.
- You have a 20-pack-year or more smoking history.
- You are in reasonably good health, without any symptoms of lung cancer.
Learn more about the Lung Cancer Screening Guideline
The number of years since quitting smoking is no longer part of the criteria for lung cancer screening. That means a person who used to smoke with at least a 20 pack-year history, whether they quit yesterday or 20 years ago, is considered to have a high risk for developing lung cancer and should be recommended for a yearly LDCT.

Treatment Studies
Survivorship Studies
More Lung Cancer Research Stories
Lung Cancer News
ACS Pivotal Studies
ACS Research Professor News Stories
We Fund Cancer Researchers Across the US
The American Cancer Society funds scientists who conduct research about cancer at medical schools, universities, research institutes, and hospitals throughout the United States. We use a rigorous and independent peer review process to select the most innovative research projects proposals to fund.
Stats on the left are as of October 17, 2025.