Your gift is 100% tax deductible.
Your Breast Pathology Report: Breast Cancer
Biopsy samples taken from your breast are studied by a doctor with special training, called a pathologist. After testing the samples, the pathologist creates a report on what was found. Your doctors will use this report to help manage your care.
- Terms you might see if cancer is found in the breast biopsy samples
- Breast cancer grade
- Stage (extent) of breast cancer
- Lymph node tests
- Estrogen receptor (ER) or progesterone receptor (PR) status
- HER2/neu or HER2 status
- Benign (non-cancerous) findings that also might be in the report
- Atypical or pre-cancer changes that also might be in the report
- Microcalcifications or calcifications
- Margins or ink
- Other lab tests that might be done on breast (or lymph node) biopsy samples
- What if my doctor asks that a special molecular test be done on my biopsy sample?
The information here is meant to help you understand some of the medical terms you might see in your pathology report after a breast biopsy, which might be a needle biopsy or a surgical (open) biopsy.
In a needle biopsy, a hollow needle is used to remove samples from an abnormal area in your breast. In some situations, a surgical biopsy might be needed. This can be either an incisional biopsy, in which only part of an abnormal area is removed, or an excisional biopsy, which removes the entire abnormal area, often with some of the surrounding normal tissue. An excisional biopsy is much like a type of breast-conserving surgery called a lumpectomy.
Terms you might see if cancer is found in the breast biopsy samples
Carcinoma or adenocarcinoma
Carcinoma is a term used to describe a cancer that begins in the lining layer (epithelial cells) of organs like the breast. Nearly all breast cancers are carcinomas. Most of these are a type of carcinoma that starts in glandular tissue, which is called an adenocarcinoma.
Infiltrating or invasive carcinoma
These terms mean that the cancer has grown (invaded) beyond the lining layer of cells in which it started, so it is a true cancer and not a pre-cancer (carcinoma in situ).
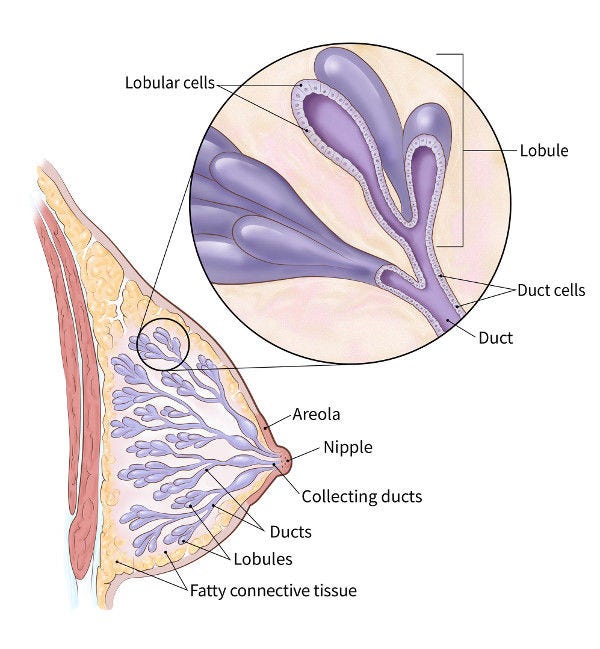
The normal breast is made of tiny tubes (ducts) that end in a group of sacs (lobules), which is where milk is made. Most breast cancers start in the cells lining the ducts or lobules.
As long as the carcinoma (cancer) cells are still confined to the breast ducts or lobules, without breaking out and growing into surrounding tissue, this is considered an in-situ carcinoma (also known as carcinoma in situ, or CIS). For more on CIS, see Your Breast Pathology Report: Ductal Carcinoma In Situ (DCIS) and Your Breast Pathology Report: Lobular Carcinoma In Situ (LCIS).
If the carcinoma cells have grown beyond the ducts or lobules, this is called an invasive or infiltrating carcinoma. In an invasive carcinoma, the tumor cells can grow outside the breast or spread (metastasize) to other parts of your body.
Invasive ductal carcinoma, invasive lobular carcinoma, or carcinoma with ductal and lobular features
The 2 main types of breast carcinomas are invasive ductal carcinoma and invasive lobular carcinoma, which is based on how they look under the microscope. (There are also some special types – see below.) In some cases, the tumor can have both ductal and lobular features, in which case it is called a mixed ductal and lobular carcinoma (or carcinoma with ductal and lobular features).
Invasive ductal carcinoma might also be called invasive mammary carcinoma of no special type. It is the most common type of breast carcinoma.
Both invasive ductal carcinomas and invasive lobular carcinomas start in the cells lining the ducts and lobules in the breast. In general, invasive lobular and invasive ductal carcinomas of the breast aren’t treated differently.
Carcinoma with tubular, mucinous, cribriform, or micropapillary features
These are different types of invasive ductal carcinoma that can be identified under the microscope.
- Tubular, mucinous, and cribriform carcinomas are "special types" of well-differentiated cancers that often have a better prognosis (outlook) than the more common type of invasive ductal carcinoma (or "invasive mammary carcinoma of no special type").
- Micropapillary carcinoma is a type of invasive breast carcinoma that often has a worse prognosis.
In some situations, different treatments might be recommended for these types of breast cancer.
Since some breast cancers are made up of more than one type, the entire tumor must be removed (by lumpectomy or mastectomy) in order to know what types your tumor contains. A needle biopsy doesn’t give enough information to guide treatment.
Vascular, lymphovascular, or angiolymphatic invasion
If cancer cells are seen in small blood vessels or lymph vessels (lymphatics) within the tumor, it is called vascular, angiolymphatic, or lymphovascular invasion.
When cancer is growing in these vessels, there is an increased risk that it has spread outside the breast. If your report doesn’t mention this type of invasion, it means it isn’t there. Even if it is there, it doesn’t always mean that your cancer has spread. How this finding might affect your treatment is best discussed with your doctor.
Breast cancer grade
When breast cancer is found, the pathologist looks for certain features that can help predict how likely the cancer is to grow and spread. These features include:
- The arrangement of the cells in relation to each other
- If the cells form tubules (gland formation)
- How much the cells look like normal breast cells (nuclear grade)
- How many of the cancer cells are dividing (mitotic count)
These features taken together determine the grade of the cancer. This can be expressed in different ways.
If the cancer is described as well differentiated, moderately differentiated, or poorly differentiated…
These terms are used to describe how closely the cancer cells and their arrangements look like those of normal, mature breast cells.
- Well-differentiated carcinomas have relatively normal-looking cells that do not appear to be growing rapidly and are arranged in small tubules for ductal cancer and cords for lobular cancer. These cancers tend to grow and spread slowly and to have a better prognosis (outlook).
- Moderately differentiated carcinomas have cells and growth patterns that look a little more abnormal.
- Poorly differentiated carcinomas lack normal features. They tend to grow and spread faster and to have a worse prognosis.
Histologic grade, Nottingham grade, or Elston grade
This is another way to express how normal or abnormal the cancer cells and their growth patterns appear. Different features (gland formation, nuclear grade, and mitotic count) are given numbers based on how they look, and then these are added to assign the grade.
- If the numbers add up to 3 to 5, the cancer is grade 1 (well differentiated).
- If they add up to 6 or 7, it means the cancer is grade 2 (moderately differentiated).
- If they add up to 8 or 9, it means the cancer is grade 3 (poorly differentiated).
Stage (extent) of breast cancer
The stage of a breast cancer is based on the size of the tumor and if the cancer has spread, as well as certain other characteristics such as the tumor grade (see above), estrogen receptor (ER) and progesterone receptor (PR) status, and HER2 status.
The standard staging system for breast cancer relies mainly on 3 key pieces of information known as TNM, where:
- T stands for the main (primary) tumor
- N stands for spread to nearby lymph nodes
- M stands for metastasis (spread to distant parts of the body)
The T category (T0, Tis, T1, T2, T3, or T4) is based on the size of the tumor and whether it has reached the skin over the breast or the chest wall under the breast. Higher T numbers mean a larger tumor and/or wider spread to tissues near the breast. (Tis is carcinoma in situ.) Since the entire tumor must be removed to learn the T category, needle biopsy results do not show this information.
The N category (N0, N1, N2, or N3) indicates if the cancer has spread to lymph nodes near the breast and, if so, how many lymph nodes are affected. Higher numbers after the N indicate more lymph node involvement by cancer. If no nearby lymph nodes were removed to be checked for cancer spread, the report may list the N category as NX, where the letter X is used to mean that the information is not available.
The M category (M0, M1) is usually based on the results of lab and imaging tests, and is not normally part of the pathology report from breast cancer surgery. In a pathology report, the M category is often left off or listed as MX (again, the letter X means that the information is not available).
If the cancer is staged after it is removed by surgery and reviewed by the pathologist, the letter p (for pathological) may appear before the T and N letters – for example, pT1, pN0, etc.
Once the T, N, and M categories, the tumor grade, and ER, PR, and HER2 status have been determined, this information is combined to give the cancer an overall stage. Stages are expressed in Roman numerals from stage I (the least advanced) to stage IV (the most advanced). Non-invasive cancer (carcinoma in situ) is listed as stage 0.
Detailed information on staging can be found in Stages of Breast Cancer. Talk with your doctor about the stage of your cancer and what it might mean for you.
Lymph node tests
If breast cancer spreads, it often goes first to the nearby lymph nodes under the arm (axillary lymph nodes). If any of your underarm lymph nodes were enlarged (found either on a physical exam or with an imaging test like an ultrasound or mammogram), they may be biopsied at the same time as your breast tumor.
Needle biopsy: One way to get a sample of cells from a lymph node is by using a thin, hollow needle. The sample is then checked for cancer cells and, if they’re found, to see what type of cancer cells they are.
Surgery: In surgery meant to treat breast cancer, lymph nodes under the arm may be removed. These lymph nodes will be looked at under the microscope to see if they contain cancer cells. The results might be reported as the number of lymph nodes removed and how many of them contained cancer (for example, 2 of 15 lymph nodes contained cancer).
Lymph node spread affects the stage of the cancer (see above) as well as a person’s prognosis (outlook). Your doctor can talk to you about what these results might mean for you.
If the report mentions a sentinel lymph node (or nodes)…
In a sentinel lymph node biopsy, the surgeon finds and removes the first lymph node(s) to which a tumor drains. This lymph node, known as the sentinel node, is the one most likely to contain cancer cells if they have started to spread. This procedure may be done during surgery for breast cancer. It is a way to check for the spread of cancer to underarm lymph nodes without needing to remove as many of them.
Once the sentinel lymph node is removed, it is checked to see if it contains cancer cells. If there is no cancer in the sentinel node(s), it's very unlikely that the cancer has spread to other lymph nodes, so no further lymph node surgery is needed.
If a sentinel lymph node does contain cancer, your report will say that cancer was present in the lymph node. It may also say how large the deposit of cancer cells is. In some cases, if cancer is found in a sentinel lymph node, you may then also need further treatment such as surgery to remove more underarm lymph nodes or radiation therapy to the underarm region. You should discuss this with your doctor.
If the report mentions isolated tumor cells in a lymph node…
This means there are only small numbers of cancer cells in the lymph node, which are either seen with a routine microscopic exam or with special tests. Isolated tumor cells do not affect your stage or change your treatment.
If the report mentions pN0(i+) or pN0(mol+)…
pN0(i+) means that isolated tumor cells were found in a lymph node using routine or special stains.
pN0(mol+) means that isolated tumor cells could only be detected in a lymph node by using very sensitive molecular tests.
If the report mentions micrometastases in a lymph node…
This means that there are more cancer cells in the lymph node than with isolated tumor cells, but these groups are still smaller than regular cancer deposits.
If micrometastases are present, the N category is listed as pN1mi. This can affect the stage of your cancer, so it might change what treatments you need. Talk to your doctor about what this finding might mean for you.
Estrogen receptor (ER) or progesterone receptor (PR) status
Receptors are proteins on cells that can attach to certain substances, such as hormones, in the blood. Normal breast cells and some breast cancer cells have receptors that attach to the hormones estrogen and progesterone. These hormones often fuel the growth of breast cancer cells.
An important step in evaluating breast cancer is to test cancer cells removed during the biopsy (or surgery) to see if they have estrogen and progesterone receptors. Cancer cells may contain neither, one, or both of these receptors. Breast cancers that have estrogen receptors are referred to as ER-positive (or ER+) cancers, while those with progesterone receptors are called PR-positive (or PR+) cancers. Hormone receptor-positive cancers tend to have a better prognosis (outlook) and are much more likely to respond to hormone therapy than cancers without these receptors.
All breast cancers and ductal carcinoma in situ (DCIS), but not lobular carcinoma in situ (LCIS), should be tested for these hormone receptors.
Results for ER and PR are reported separately, and they might be reported in different ways:
- Negative, weakly positive, or positive
- Percent positive
- Percent positive and whether the staining is weak, moderate, or strong
How the results of these tests might affect your treatment choices is best discussed with your doctor.
HER2/neu or HER2 status
Some breast cancers have too much of a protein called HER2/neu (often just shortened to HER2), which helps them grow. The HER2 gene instructs the cells to make this protein. Tumors with higher levels of HER2 are referred to as HER2-positive.
In HER2-positive breast cancers, the cancer cells have too many copies of the HER2 gene, resulting in higher than normal amounts of the HER2 protein. These cancers tend to grow and spread more quickly than other breast cancers, but they are also more likely to respond to drugs that target the HER2 protein.
The biopsy or surgery sample is usually tested for HER2 in 1 of 2 ways:
- Immunohistochemistry (IHC): In this test, special antibodies that will stick to the HER2 protein are applied to the sample, which cause cells to change color if they have higher levels of HER2 protein. This color change can be seen under a microscope. The test results are reported as 0, 1+, 2+, or 3+.
- Fluorescence in situ hybridization (FISH): This test uses fluorescent pieces of DNA that specifically stick to copies of the HER2 gene in cells, which can then be counted under a special microscope.
While the FISH test is thought to be more accurate than IHC, it is more expensive, and it takes longer to get the results. Often the IHC test is used first:
If the IHC result is 0, the cancer is considered HER2-negative. These cancers do not respond to treatment with drugs that target HER2.
- If the IHC result is 1+, the cancer is also considered HER2-negative. While these cancers do not usually respond to treatment with drugs that target HER2, newer research shows that certain HER2 drugs might help in some cases (see below).
- If the IHC result is 2+, the HER2 status of the tumor is not clear and is called "equivocal." This means that the HER2 status needs to be tested with FISH to clarify the result.
- If the test comes back as 3+, the cancer is HER2-positive, so treatment with drugs that target HER2 might be helpful.
Some breast cancers that have an IHC result of 1+ or an IHC result of 2+ along with a negative FISH test might be called HER2-low cancers. Treatment of these breast cancers is still being studied, but they appear to benefit from certain HER2-targeted drugs.
A newer type of test, known as chromogenic in situ hybridization (CISH), works similarly to FISH, by using small DNA probes to count the number of HER2 genes in breast cancer cells. This test looks for color changes (not fluorescence) and doesn't require a special microscope, which might make it less expensive than FISH. Right now, it is not used as much as IHC and FISH.
How the results of these tests might affect your treatment is best discussed with your doctor.
Benign (non-cancerous) findings that also might be in the report
- Usual ductal hyperplasia
- Adenosis
- Sclerosing adenosis
- Radial scar
- Complex sclerosing lesion
- Papillomatosis
- Papilloma
- Apocrine metaplasia
- Cysts
- Columnar cell change
- Collagenous spherulosis
- Duct ectasia
- Fibrocystic changes
- Flat epithelial atypia
- Columnar alteration with prominent apical snouts and secretions (CAPSS)
All of these are non-cancerous (benign) changes that the pathologist might have seen. They are not important when seen on a biopsy result that also shows invasive breast cancer.
Atypical or pre-cancer changes that also might be in the report
- Atypical ductal hyperplasia (ADH)
- Atypical lobular hyperplasia (ALH)
- Ductal carcinoma in situ (DCIS)
- Intraductal carcinoma
- Lobular carcinoma in situ (LCIS)
- In-situ lobular carcinoma
These are types of atypical or pre-cancer changes that can sometimes be seen on breast biopsy. If they are found in a needle biopsy that also shows invasive cancer, they typically are not important.
They may, however, need to be removed completely as a part of treatment. If they are seen on an excisional biopsy at or near a margin (see below about margins), more breast tissue may need to be removed (even if all of the invasive cancer was taken out).
For more on these conditions, see Your Breast Pathology Report: Ductal Carcinoma in Situ (DCIS), Your Breast Pathology Report: Lobular Carcinoma in Situ (LCIS), or Your Breast Pathology Report: Atypical Hyperplasia.
Microcalcifications or calcifications
Microcalcifications or calcifications are small calcium deposits that can be found in both non-cancerous and cancerous breast lesions. They can be seen both on mammograms and under the microscope.
Because certain calcifications can be found in areas containing cancer, their presence on a mammogram may lead to a biopsy of the area. Once the biopsy is done, the pathologist looks at the removed tissue to be sure that it contains calcifications. If the calcifications are there, the doctor knows that the biopsy sampled the correct area (the abnormal area on the mammogram).
Margins or ink
When an entire tumor (and some surrounding normal breast tissue) is removed, the outside edges (or margins) of the specimen are coated with ink, sometimes even with different colors of ink on different sides of the specimen. This helps the pathologist know which edge of the tumor they’re looking at.
The pathologist looks at slides of the tumor to see how close the cancer cells are to the ink (the edges or margins of the specimen). If cancer cells are touching the ink (called positive margins), it can mean that some cancer was left behind, and more surgery or other treatments might be needed. Sometimes, though, the surgeon has already removed more tissue (at surgery) to help make sure that this isn’t needed.
Sometimes, all of the invasive cancer is removed, but there may be pre-cancer or another serious condition at or near the margin, such as ductal carcinoma in situ (DCIS).
If your pathology report shows positive margins, your doctor will talk to you about what treatment is best.
Other lab tests that might be done on breast (or lymph node) biopsy samples
E-cadherin
E-cadherin is a test that might be used to help determine if the tumor is ductal or lobular. (The cells in invasive lobular carcinomas are often negative for E-cadherin.) If your report doesn’t mention E-cadherin, it means that this test wasn’t needed to tell what type of cancer you have.
D2-40 (podoplanin) or CD34
D2-40 and CD34 are special tests that might be used to help identify the different types of vascular invasion in a tumor (see above). These tests are not always needed.
Ki-67
Ki-67 is a way to measure how fast the cancer cells are growing and dividing. Higher values for Ki-67 (typically over 30%) mean that many cells are dividing, so the cancer is likely to grow and spread more quickly.
High molecular weight cytokeratin (HMWCK), CK903, CK5/6, p63, muscle specific actin, smooth muscle myosin heavy chain, calponin, or keratin
These are special tests that might be used to help diagnose invasive breast cancer or to identify cancer in lymph nodes. Not all biopsies need these tests. Whether or not your report mentions these tests has no bearing on the accuracy of your diagnosis.
What if my doctor asks that a special molecular test be done on my biopsy sample?
Molecular tests (also known as gene expression profiling or genomic tests) are special tests that look at the activity of many different genes at once. Examples of these tests include:
- Oncotype DX
- MammaPrint
- Prosigna
- Breast Cancer Index (BCI)
These tests might be done in some situations to help predict the prognosis (outlook) for people with breast cancer or to determine if certain treatments are likely to be helpful, but not everyone needs these tests.
If one of these tests is done on your biopsy specimen, ask your doctor to explain what the results mean. The results will not affect your diagnosis, but they might affect your treatment options.
- Written by

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
Last Revised: July 7, 2023
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.



