Your gift is 100% tax deductible.
Ablation and Embolization for Colorectal Cancer
Ablation and embolization are sometimes used to treat colorectal cancer that has spread to other parts of the body, such as the liver or lungs.
When are ablation and embolization used?
When colon or rectal cancer has spread and there are a few small tumors in the liver or lungs, these metastases can sometimes be removed by surgery or destroyed by other techniques, such as ablation or embolization.
When all of the primary cancer in the colon or rectum can be removed with surgery, ablation or embolization might be used to destroy small tumors in other places in the body.
Ablation and embolization might also be good options for people whose metastatic tumors come back after surgery, whose cancer can’t be cured with surgery, or who can’t have surgery for other reasons. This might help a person live longer. It can also help treat problems the cancer is causing, like pain.
In most cases, patients don’t need to stay in the hospital for these treatments.
Ablation
Ablation techniques are used to destroy small tumors (less than 4 cm across) instead of removing them with surgery. There are many different types of ablation techniques. They can be used to treat tumors in other places, too.
Radiofrequency ablation (RFA)
Radiofrequency ablation is one of the most common methods to treat cancer that has spread to the liver. It uses high-energy radio waves to kill cancer cells. A CT scan or ultrasound is used to guide a thin, needle-like probe through the skin and into the tumor. An electric current is then sent to the tip of the probe, releasing high-frequency radio waves that heat the tumor and destroy the cancer cells.
Microwave ablation (MWA)
The microwave ablation method is used to treat cancer that has spread to the liver. Imaging tests are used to guide a needle-like probe into the tumor. Electromagnetic microwaves are then sent through it to create high temperatures that kill the cancer quickly. This treatment has been used to treat larger cancers (up to 6 cm across).
Percutaneous ethanol ablation (PEI) or Alcohol ablation
Percutaneous ethanol injection destroys the cancer cells by injecting concentrated alcohol into the tumor. This is usually done through the skin using a needle, which is guided by ultrasound or CT scans. Sometimes multiple treatments of PEI may be needed to treat the whole tumor.
Cryoablation
Cryoablation destroys the tumor by freezing it with a thin metal probe. The probe is guided through the skin and into the tumor using ultrasound. Then very cold gas (usually liquid nitrogen or argon gas) is passed through the end of the probe to freeze the tumor, killing the cancer cells. This method can treat larger tumors than the other ablation techniques, but sometimes general anesthesia (drugs used to put the patient into a deep sleep) is needed. Treatment can be repeated as needed to kill all the cancer cells.
Side effects of ablation therapy
Possible side effects after ablation therapy include:
- Abdominal (belly) pain
- Infection in the liver
- Fever
- Bleeding into the chest cavity or abdomen
- Abnormal liver tests.
Serious complications are rare, but they are possible.
Embolization
Embolization is used to treat tumors in the liver. In an embolization procedure, a substance is injected directly into an artery in the liver to block or reduce the blood flow to the tumor.
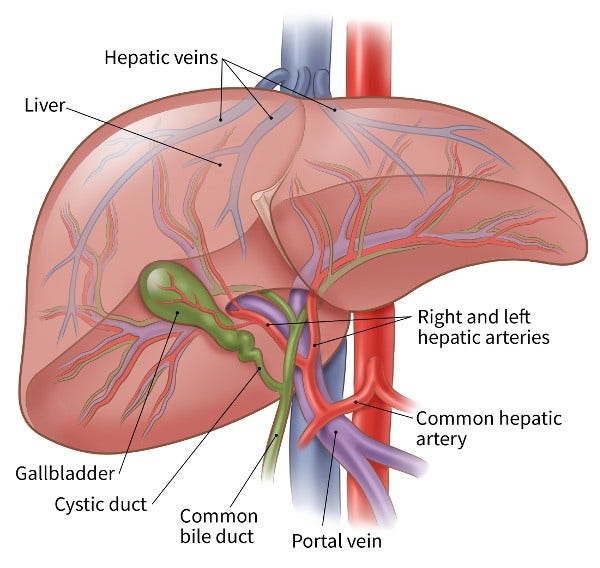
The liver is special in that it has 2 blood supplies. Most normal liver cells get blood from the portal vein, but cancer cells in the liver usually get their blood supply from the hepatic artery. Blocking the part of the hepatic artery that feeds the tumor helps kill the cancer cells, and it leaves most of the healthy liver cells unharmed because they get their blood supply from the portal vein.
Embolization can be used to treat tumors larger than 5 cm (about 2 inches) across that are often too big to be treated with ablation. It can also be used along with ablation. Embolization does reduce some of the blood supply to the normal liver tissue, so it may not be a good option for patients with liver damage from diseases like hepatitis or cirrhosis.
There are 3 main types of embolization procedures used to treat colon or rectal cancer that has spread (metastasized) to the liver:
- Arterial embolization is also called trans-arterial embolization or TAE. In this procedure, a catheter (a thin, flexible tube) is put into an artery through a small cut in the inner thigh and eased up into the hepatic artery in the liver. A dye is usually injected into the blood to help the doctor watch the path of the catheter using x-ray pictures. Once the catheter is in the right place, small particles are injected into the artery to plug it up, blocking oxygen and key nutrients from the cancer.
- Chemoembolization (also called trans-arterial chemoembolization or TACE) combines arterial embolization with chemotherapy. TACE is done by giving chemotherapy through a catheter that’s put right into the artery that feeds the tumor, then plugging up the artery so the chemo can stay close to the tumor. Multiple treatments may be given over 4 to 6 weeks.
- Radioembolization combines embolization and radiation therapy. This is done by injecting tiny beads (called microspheres) coated with radioactive yttrium-90 (Y-90) into the hepatic artery. The beads lodge in the blood vessels near the tumor where they give off small amounts of radiation to the tumor site for several days. The radiation travels a very short distance, so its effects are limited mainly to the tumor.
Possible side effects of embolization
Possible side effects after embolization include:
- Abdominal (belly) pain
- Infection in the liver
- Fever
- Gallbladder inflammation
- Blood clots in the main blood vessels of the liver
- Abnormal liver tests
Because healthy liver tissue can be affected, there is a risk that liver function will get worse after embolization. This risk is higher if a large branch of the hepatic artery is embolized. Serious complications are not common, but they are possible.
- Written by
- References

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
Aykut B, Lidsky ME. Colorectal Cancer Liver Metastases: Multimodal Therapy. Surg Oncol Clin N Am. 2023 Jan;32(1):119-141. doi: 10.1016/j.soc.2022.07.009. Epub 2022 Nov 3. PMID: 36410912.
Boas FE, Bodei L, Sofocleous CT. Radioembolization of Colorectal Liver Metastases: Indications, Technique, and Outcomes. J Nucl Med. 2017;58(Suppl 2):104S-111S.
Kelly SR and Nelson H. Chapter 75 – Cancer of the Rectum. In: Niederhuber JE, Armitage JO, Dorshow JH, Kastan MB, Tepper JE, eds. Abeloff’s Clinical Oncology. 6th ed. Philadelphia, Pa. Elsevier: 2020.
Lawler M, Johnston B, Van Schaeybroeck S, Salto-Tellez M, Wilson R, Dunlop M, and Johnston PG. Chapter 74 – Colorectal Cancer. In: Niederhuber JE, Armitage JO, Dorshow JH, Kastan MB, Tepper JE, eds. Abeloff’s Clinical Oncology. 6th ed. Philadelphia, Pa. Elsevier: 2020.
National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology: Colon Cancer. V.1.2024. Accessed at https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf on Jan 29, 2024.
National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology: Rectal Cancer. V.1.2024. Accessed at https://www.nccn.org/professionals/physician_gls/pdf/rectal.pdf on Jan 29, 2024.
Uhlig J, Lukovic J, Dawson LA, Patel RA, Cavnar MJ, Kim HS. Locoregional Therapies for Colorectal Cancer Liver Metastases: Options Beyond Resection. Am Soc Clin Oncol Educ Book. 2021 Mar;41:133-146. doi: 10.1200/EDBK_320519. PMID: 34010047.
Last Revised: January 29, 2024
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.



