Your gift is 100% tax deductible.
How Cancer Can Affect Sexual Desire in Men
When you go through cancer treatment, it’s common to lose interest in sex, at least for a while. Treatment can cause physical and emotional changes, and some of these changes might affect your desire for sex.
These changes might also make it harder to have sex or be intimate in the same ways as you did before cancer.
For most people, this loss of sexual desire is temporary. Once you finish treatment and have recovered, your desire for sex and intimacy will most likely return. But if you continue to have problems, there are ways to deal with these changes so that you can have a satisfying sex life.
- How cancer and treatment can affect sexual desire
- Side effects and sexual desire
- Hormone therapy and sex drive
- Emotions and sex after cancer
- Specific cancers and treatments that can affect sexual desire
- Feeling good about yourself and feeling good about sex
- Overcoming anxiety about sex
- Making sex more comfortable
- Getting professional help
- Learn more
How cancer and treatment can affect sexual desire
There are many reasons cancer and cancer treatment can affect your desire for sex.
If you are worried, depressed, nauseous (sick to your stomach), having pain, or experiencing fatigue, you may not feel like having sex. Cancer treatments that disturb the normal hormone balance in your body can lessen your desire for sex as well. You also might not feel like sex is a priority while you’re getting treated.
If you continue to have problems, think about working with a therapist who has experience working with people with cancer. Your cancer care team should be able to refer you.
The information below describes common sexual problems faced by adult men (or people with male reproductive organs*) after certain types of cancer treatment. You might have problems or needs that aren’t addressed here. Your cancer care team can help you manage your specific situation.
*To learn more about the gender terms used here, and how to start the conversation with your cancer care team about gender identity and sexual orientation, see Gender Identity, Sexual Orientation, and Cancer Treatment.
Side effects and sexual desire
Some side effects of cancer and cancer treatment can lower your desire for sex.
Pain
Pain in any part of your body can make you feel worried, depressed, or easily discouraged. If you have these feelings, you may find it hard to get excited about sexual activity.
Some men have pain in their genitals during sex.
- Ejaculation may cause pain if your prostate or urethra is irritated from cancer treatment.
- Orgasm may cause pain if you have scar tissue in your abdomen (belly) and pelvis after surgery (such as for colon cancer).
- Pain in the penis as it becomes erect is less common.
Tell your doctor right away if you have any pain in your genital area.
Other side effects
Other side effects that can lower your desire for sex include:
- Fatigue
- Nausea and vomiting
- Changes in how you look, such as rashes, hair loss, scars, or an ostomy
Hormone therapy and sex drive
Cancer treatments that lower your hormone levels can reduce your desire for sex.
Testosterone can fuel the growth of prostate cancer. If prostate cancer has spread beyond the gland, treatment often includes hormone therapy to lower your testosterone levels. The goal of hormone therapy is to starve the prostate cancer cells of testosterone. This slows the growth of the cancer.
Your testosterone levels can be lowered by:
- Medicine that helps prevent testosterone from being made, or
- Surgery to remove your testicles (orchiectomy)
Both treatments affect your testosterone levels, so they have many of the same kinds of sexual side effects.
A decreased desire for sex (libido) is the most common sexual side effect of hormone treatment.
Hormone therapy can also cause physical changes, such as:
- Loss of muscle mass
- Weight gain
- Some growth of breast tissue
Psychological effects of hormone therapy
Some men who get hormone therapy to lower testosterone report feeling less masculine. While hormone therapy for prostate cancer may decrease your desire for sex, it doesn’t change who you find attractive.
Hormone therapy has also been linked to depression. If you feel sad or depressed, talk with your urologist or cancer care team about how it can be managed.
Some studies suggest hormone therapy for prostate cancer may also lead to problems with thinking, concentration, and/or memory.
Managing the side effects of hormone therapy
Ask your cancer care team about possible side effects from hormone therapy and how you might manage them.
For instance, an exercise program may help you limit muscle loss, weight gain, and tiredness. Talk with your cancer care team about an exercise program or ask to be referred to a physical therapist who can help you come up with a plan.
Emotions and sex after cancer
Your emotions about cancer and treatment can also affect your interest in sex and your ability to be intimate with your partner. You might feel:
- Afraid your cancer will come back
- Sad, frustrated, or powerless
- Bad about changes in your body
- Stressed, depressed, or anxious
Your partner might have many of these same emotions. Talk with each other about your feelings and concerns, including how these feelings might affect your sexual desire. Keeping these feelings to yourself can get in the way of being intimate, both physically and emotionally.
You might also want to talk with your doctor or cancer care team if your feelings are getting in the way of being intimate with a partner. They will have resources to help you, or they can refer you to a counselor or sex therapist.
Specific cancers and treatments that can affect sexual desire
Any type of cancer or cancer treatment can affect your desire for sex, at least for a while. But some cancers and treatments are more likely to cause long-term changes to the way you experience sex.
If you have cancer of the penis or the bottom end of the urethra, the treatment may be to remove part or all of your penis (penectomy). These operations can have a major effect on self-image and sex life.
Penile-sparing techniques
Penile-sparing techniques are used as often as possible. These include local treatments and limited surgeries. The goal is to treat the cancer while also saving as much of your penis as possible to preserve sexual function, the way the penis looks, and the ability to urinate while standing up.
In these cases, most men can still reach orgasm and have a normal orgasm.
Total penectomy
A total penectomy removes your entire penis, including the base that extends into your pelvis. The surgeon creates a new way for urine to leave your body through an opening between your scrotum and anus (the outside opening of the rectum).
You can still control your urination because the “on-off” valve in the urethra is above the level of the penis.
Sex and intimacy after a total penectomy
Men who’ve had a total penectomy can still feel pleasure from touching of the genital area, such as the scrotum and inner thighs. New approaches to sexual pleasure can be explored, and working with a sex therapist may be helpful. Ask your cancer care team for suggestions of a sex therapist you could work with.
Treatment for testicular cancer usually means removing one or both testicles, or testes (orchiectomy). Although some men are not upset about the loss of a testicle, others may fear a partner’s reaction.
Since this operation also removes the epididymis (the narrow, coiled tube above the testicle), that side of the scrotum looks and feels empty. If you would like a more natural look, you can have a testicular prosthesis put in your scrotum during surgery. You can ask for a prosthesis that matches your remaining testicle.
If you have prostate surgery, your penis may be shorter than before. This might happen because the surgery affects the nerves that control your erections. Blood flow changes, scarring, and changes in penile tissue that can happen if you can’t have erections may also play a role.
There’s no known way to prevent or treat penile shrinkage. But early penile rehabilitation might help decrease this shortening. Vacuum devices might also be helpful.
You can learn more about these devices in How Cancer Affects Erections.
Surgery or radiation therapy for head and neck cancers can lead to changes in how you look and breathe. These changes may affect how you feel about being intimate with another person.
Appearance changes
Some cancers of the head and neck are treated by removing part of the bone structure of the face. This can change your appearance. Surgery on the jaw, mouth, or tongue can also change the way you look and talk. Facial reconstruction can help you regain a more normal look and clearer speech.
Laryngectomy and tracheostomy
Some people with head and neck cancer will need to have part of their airway removed.
- A laryngectomy is surgery that removes part or all of your voice box (larynx). A total laryngectomy (and some partial laryngectomies) leaves you unable to talk in the usual way. Since your larynx is next to the windpipe that connects your mouth and lungs, you might need a tracheostomy.
- A tracheostomy creates a new airway. Instead of breathing through your mouth and nose, you will breathe through a stoma (opening or hole) in the front of your neck. A tracheostomy might be created during laryngectomy surgery. It can be temporary or permanent.
Adjusting to sex and intimacy with a stoma
If you are uncomfortable about the way your stoma looks, a scarf, ascot tie, or turtleneck can help hide it. During sex, a partner may at first be startled by breath that hits at an unexpected spot. This can take some getting used to.
You might also have food odors coming from your stoma. You can lessen this by avoiding garlic or spicy foods and by wearing cologne or after-shave lotion.
Sometimes, problems speaking can make it hard to communicate during sex. If you learn to speak using your esophagus, this could make talking during sex less of an issue. A speech aid or electronic voice box also works well.
Limb amputation
Treatment for some cancers can include surgically removing (amputating) a limb, such as an arm or leg.
If you’ve lost a limb, you may wonder whether to wear your artificial limb (prosthesis) during sex. Sometimes the prosthesis can help with positioning and ease of movement. Talk with your partner about what works best for the two of you.
Urostomy, colostomy, or ileostomy
An ostomy allows waste to leave your body through an opening (stoma) in the skin and into a pouch that you can empty.
- A urostomy takes urine through a new passage and sends it out through an opening on your belly (abdomen).
- A colostomy or ileostomy gets rid of stool (poop) from your intestines through an opening on your belly. In an ileostomy, the opening is made with the part of the small intestine called the ileum. A colostomy is made with a part of the large intestine called the colon.
Adjusting to sex and intimacy with an ostomy
There are ways to reduce the effect an ostomy has on your sex life. Make sure your appliance (pouch system) fits well. Check the seal and empty your ostomy bag before sex. This will reduce the chance of a leak.
Learn more in Ostomies.
Feeling good about yourself and feeling good about sex
Sometimes friends and partners withdraw when a person has cancer. This can be out of fear or uncertainty. It can help to talk with your partner about how each of you is feeling.
Sexual touching between you and your partner is always possible. It just may be different than before you got treated for cancer. It may be easy to forget this, especially if you’re both feeling down or have not had sex in a while.
Keep in mind that you might need extra help with the changes caused by cancer. Counseling and sex therapy may be good options.
Overcoming anxiety about sex
You might find it hard to be as spontaneous as you used to be. Try setting up time with your partner to relax, enjoy one another’s company, and talk about what each of you would like sexually. Just as you learned to enjoy sex when you first started having it, you can learn how to feel pleasure again during and after cancer treatment.
Masturbation is not a required step in resuming your sex life, but it might help. It can help you find out where you are tender or sore and what kind of touch you enjoy. Sharing this information can help you and your partner decide what next steps to take.
Depending on your situation, you may feel a little shy bringing up sex. It might be hard to let your partner know you would like more physical closeness or that you are anxious about having sex. But these conversations are an important step toward resuming a fulfilling sex life. So be as clear and direct as you can.
Making sex more comfortable
If you have pain or feel weak from cancer treatment, you might want to try new sex positions. Talk to your partner and learn different ways to enjoy sex that are more comfortable for you. The drawings below are some ideas for positions that may help as you resume sex.
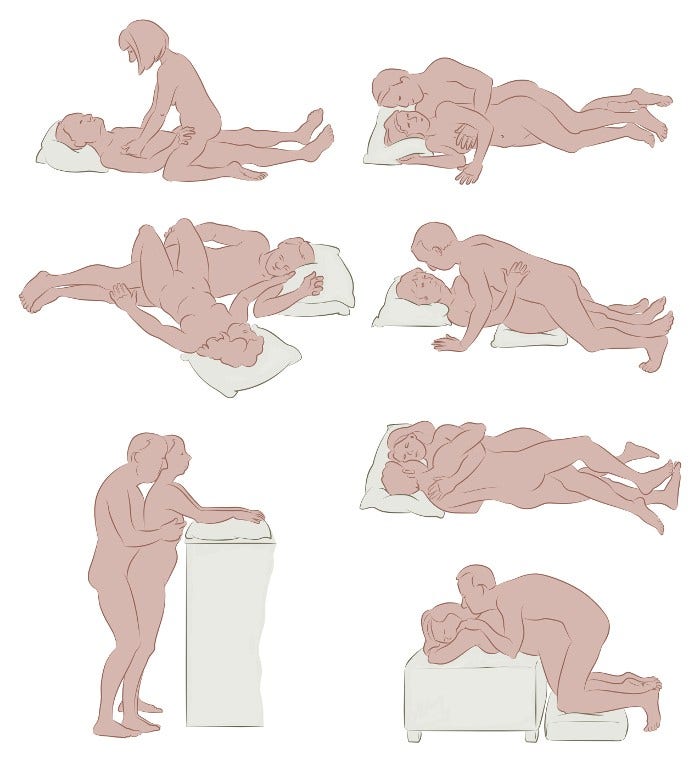
There’s no one position that’s right for everyone. You and your partner can work together to find what’s best for you. Pillows can help as supports. Keeping a sense of humor can always lighten up your efforts.
Getting professional help
Many health care professionals, including cancer doctors and nurses, have little training in sexuality issues. Depending on the problems you are having, you might be referred to a different kind of specialist.
A urologist focuses on diseases of the urinary tract and male genitals, and sexual problems. Many urologists perform surgery or order medical treatments for erection problems. They also have the special equipment that may be needed to find the cause of an erection problem.
An endocrinologist is an expert in how hormones work in the body. If the most likely cause of a sexual problem is a hormone imbalance, an endocrinologist may be able to help.
There are many different programs and specialists that can help you find the answers you need. Ask your cancer care team or primary care provider for referrals to specialists who can help you.
Counseling and sex therapy
There are also health care professionals who can help you understand and manage the emotions that affect your sex life. Options include:
- Talking with a counselor or sex therapist.
- Finding help in your community, such as a support group for men who are cancer survivors.
- Seeing a couples counselor who can help you talk about tough issues with your partner, including emotions that interfere with intimacy and sex.
Sexual rehabilitation programs
Some cancer centers have experts on staff who can assess and treat sexual problems. Ask your cancer care team if your center offers any programs or where else you can get help.
Sex therapists and other types of counselors
Sex therapy is psychotherapy or counseling that focuses on solving a sexual problem.
Sex therapists may practice in a clinic or alone. Look for a sex therapist who is a licensed mental health professional (a psychiatrist, psychologist, social worker, or psychiatric clinical nurse specialist or nurse practitioner) with special training in treating sexual problems.
Psychotherapy can help you feel better about the changes in your body, help you and your partner communicate more clearly, and give you skills to better cope with your cancer and treatment. Couples counseling may be helpful, too.
Finding a well-qualified mental health professional is important. These are some of the different types of mental health professionals:
- Psychiatrist: This is a medical doctor (an MD or DO) with a specialty in psychiatry. They should also be certified by the American Board of Psychiatry and Neurology.
- Psychologist: Most psychologists who practice alone have a doctorate in psychology (PhD or PsyD) or in education (EdD). Psychologists do not have medical degrees and don’t write prescriptions. A psychologist with a master’s degree is usually supervised by someone with a doctorate. In most states, a psychologist must be licensed. Those who practice usually have degrees in clinical or counseling psychology.
- Social worker: A social worker usually has a master’s degree in social work (MSW). Many social workers have training in mental health counseling. Licensing laws vary from state to state.
- Marriage and family counselors: Some states have a category for licensed psychotherapists called marriage and family counselors. They usually have a master’s degree in psychology or a related field, plus training in counseling.
- Psychiatric clinical nurse specialists or psychiatric nurse practitioners: This is someone with a master’s or doctorate degree in psychiatric nursing. They are licensed professionally, although their ability to prescribe medicines varies from state to state.
Finding a sex therapist or counselor
Professional societies can often give you information about their members in your area who have special training in sex therapy. These are good places to start:
- American Association of Sex Educators, Counselors, and Therapists (AASECT)
www.aasect.org
- National Association of Social Workers (NASW)
www.helpstartshere.org
You can also get a listing of professionals in your area by contacting your state’s psychological association or a state association for licensed marriage and family therapists.
The cost of counseling varies with the professional’s level of training and experience. Insurance coverage for counseling varies depending on the health insurance plan. Check with your insurance company to find out if your plan will pay for counseling and how much of the cost it will cover.
Learn more
- Written by
- References

Developed by the American Cancer Society medical and editorial content team with medical review and contribution by the American Society of Clinical Oncology (ASCO).
American Society of Clinical Oncology. Sexual Health and Cancer Treatment: Men. Cancer.net. Content is no longer available.
Calabrò RS, Cacciola A, Bruschetta D, et al. Neuroanatomy and function of human sexual behavior: A neglected or unknown issue?. Brain Behav. 2019;9(12):e01389. doi:10.1002/brb3.1389
Carter et al. Interventions to address sexual problems in people with cancer: American Society of Clinical Oncology clinical practice guideline adaptation of Cancer Care Ontario guideline. Journal of Clinical Oncology. 2018;36(5):492-513.
Dizon DS, Katz A. Overview of sexual dysfunction in male cancer survivors. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on November 4, 2024.
Emery J, Butow P, Lai-Kwon J, Nekhlyudov L, Rynderman M, Jefford M. Management of common clinical problems experienced by survivors of cancer. Lancet. 2022;399(10334):1537-1550. doi:10.1016/S0140-6736(22)00242-2
Katz A. Breaking the Silence on Cancer and Sexuality: A Handbook for Healthcare Providers. 2nd ed. Pittsburgh, PA: Oncology Nursing Society.; 2018.
Khera M. Treatment of male sexual dysfunction. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on November 4, 2024. Peters M, Pearlman A, Terry W, Mott SL, Monga V. Testosterone deficiency in men receiving immunotherapy for malignant melanoma. Oncotarget. 2021;12(3):199-208. Published 2021 Feb 2. doi:10.18632/oncotarget.27876
Richie JP. Radical prostatectomy for localized prostate cancer. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on November 11, 2024.
Rosen RC, Khera M. Epidemiology and etiologies of male sexual dysfunction. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on November 11, 2024.
Steele GS. Radical inguinal orchiectomy for testicular germ cell tumors. In, UpToDate, Post TW (Ed). Accessed at uptodate.com on December 6, 2024.
Stroie FA, Houlihan MD, Kohler TS. Sexual function in the penile cancer survivor: a narrative review. Transl Androl Urol. 2021;10(6):2544-2553. doi:10.21037/tau-20-1228
Zavattaro M, Felicetti F, Faraci D, et al. Impact of Allogeneic Stem Cell Transplantation on Testicular and Sexual Function. Transplant Cell Ther. 2021;27(2):182.e1-182.e8. doi:10.1016/j.jtct.2020.10.020
Last Revised: April 15, 2025
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.



