Your gift is 100% tax deductible.
The Role of Diet in Reducing CIPN Risk for Colon Cancer Patients
Certain types of chemotherapy for people with colon or rectal cancer increase the risk of peripheral neuropathy, but healthy eating may help lower that risk.
The Challenge
Chemotherapy-induced peripheral neuropathy (CIPN) is a significant and debilitating side effect for cancer patients receiving certain kinds of chemotherapy. Characterized by pain, numbness, and tingling in the hands and feet, CIPN drastically diminishes patients’ quality of life and may last even after the chemotherapy ends. This nerve issue may even require dose reductions or interruptions in chemotherapy, which limits the effectiveness of treatment. For individuals receiving the chemotherapy oxaliplatin as part of their treatment plan after surgery for colon cancer, the risk of developing CIPN is particularly high.
Although fewer people are being diagnosed with colon or rectal cancer since the mid-1980s, colon cancer is still one of the most common and deadly cancers worldwide. Thousands of patients depend on chemotherapy for their treatment. However, 85% of these patients experience CIPN after their first cycle of oxaliplatin. This makes research into CIPN crucial for improving patient care.
However, if side effects like CIPN become too severe, treatment must be modified or stopped altogether, and that happens far too often. Lowering the amount of chemotherapy can lead to worse outcomes, meaning patients are less likely to stay cancer-free and live longer. This problem has led researchers to search for ways to reduce CIPN while helping patients receive the full therapeutic benefit of chemotherapy.
The Research
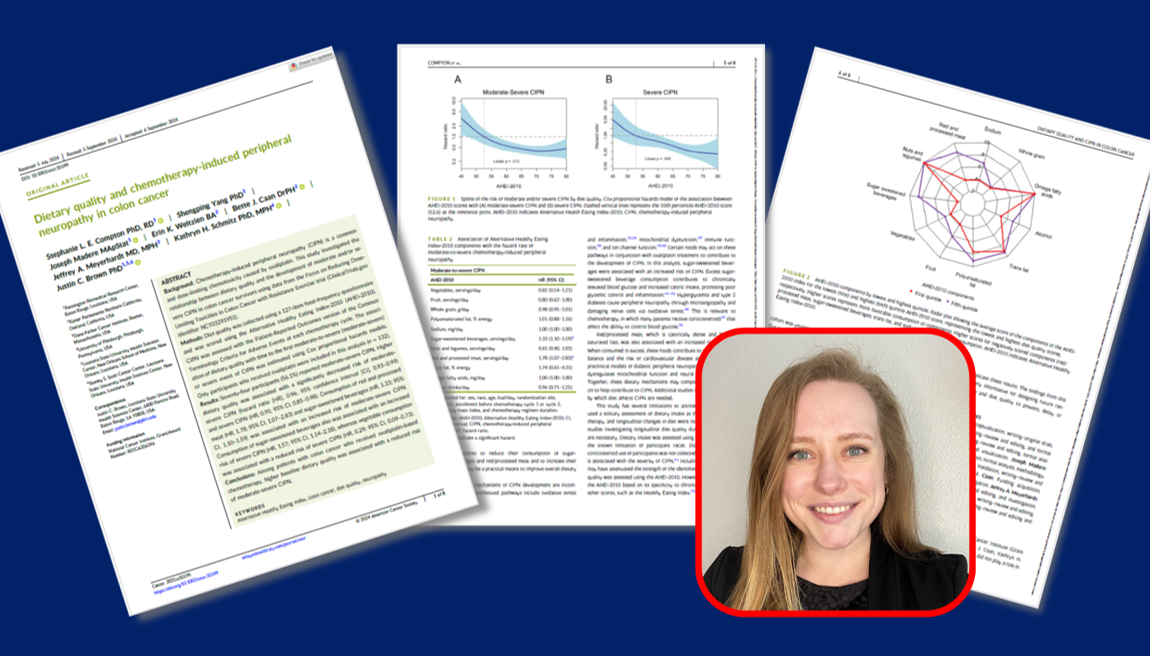
Most research on nutrition and chemotherapy-induced peripheral neuropathy (CIPN) has looked at the effects of specific vitamins, minerals, and nutrients. However, new evidence suggests that overall diet quality might help lower the risk and severity of CIPN in patients receiving platinum-based chemotherapy. In this study, American Cancer Society-funded postdoctoral fellow Stephanie Compton, PhD, RD, LDN, and her collaborators explored whether “dietary quality”—an often-overlooked factor in cancer care—plays a role the risk and severity of CIPN in colon cancer patients receiving oxaliplatin-based chemotherapy.
Using data from the FORCE (Focus on Reducing Dose-Limiting Toxicities in Colon Cancer with Resistance Exercise trial, Dr. Compton and her fellow researchers analyzed dietary information from 132 participants on oxaliplatin using a 127-item food frequency questionnaire and the Alternative Healthy Eating Index-2010 (AHEI-2010), a well-validated measure of nutritional quality that emphasizes foods and nutrients associated with chronic disease risk, including cancer. Eleven participants received oxaliplatin for stage II colon cancer and 121 participants received oxaliplatin for stage III colon cancer.
At each of their treatment cycles, patients self-reported the severity and degree of interference CIPN symptoms had on daily activities. This enabled the research team to look at how CIPN developed over time. They then used statistical analyses to assess the relationship between dietary quality and the risk of moderate-to-severe CIPN.
With the use of statistical analyses, the research team found that colon cancer patients’ dietary quality was associated with the risk of developing CIPN and associated with its severity. Specifically, they found:
- Participants had a significantly higher risk of moderate-to-severe CIPN with a low dietary quality, characterized by higher consumption of red and processed meats and sugar-sweetened beverages.
- Participants had a significantly lower risk of severe CIPN with a high dietary quality, characterized by a diet rich in vegetables
These results highlight the potential influence of diet quality on chemotherapy tolerability with oxaliplatin, offering new insights into supportive cancer care interventions and opportunities to reduce treatment side effects.
Why Does It Matter
This research is a major step forward in understanding how lifestyle factors, like diet, influence the experience of cancer treatment. While following a healthy diet has long been recommended as a key component in preventing cancer, the discovery that a higher-quality diet can reduce the risk of moderate-to-severe CIPN in colon cancer patients holds promise for improving the way cancer care is approached. Ultimately, this highlights the importance of comprehensive patient support systems that include nutritional guidance at all stages of cancer care.
Public health efforts aimed at reducing the burden of treatment-related side effects could benefit greatly from the integration of dietary recommendations into cancer care protocols. For patients, adopting healthier eating habits—such as consuming more vegetables and reducing intake of red meats and sugar-sweetened beverages—may offer a simple yet effective way to enhance their quality of life during chemotherapy.
While this study offers valuable insights, it also raises important questions for future research. Since the study focused solely on colon cancer patients undergoing a specific type of treatment, it is essential to expand investigations to include other cancer types and treatment modalities. Further research is also needed to unravel the biology behind how diet may reduce the risk of CIPN and to test these findings in larger and more diverse populations. Additionally, future studies should examine the influence of other lifestyle factors, such as physical activity and stress management, in reducing treatment side effects. Equally important is implementing strategies to improve the affordability and accessibility of healthy foods, particularly in underserved communities, where disparities continue to drive inequitable health outcomes.



