What to Know About Bariatric Surgery (Weight Loss Surgery)
Bariatric surgery (weight loss surgery) is one of the options available to some people to help with excess body weight. Bariatric surgery that leads to weight loss can help manage or even reverse some health conditions, such as diabetes and high blood pressure, and can help improve quality of life.
How does bariatric surgery work?
Bariatric surgeries are done on the stomach or intestines to cause weight loss. These surgeries work to change the stomach or intestines (or both) in a way that:
- Reduces the amount of food that a person can eat
- Changes how food is digested or absorbed
- Impacts hunger and fullness hormones
Each type of bariatric surgery takes a unique approach, but all aim to support long-term weight loss and improve health conditions related to excess body weight.
How effective is bariatric surgery?
For some types of bariatric surgery, people may lose about 25% body fat and are likely to keep it off for at least 5 years. It’s important to know that the full results of surgery might take some time. Initial weight loss may be rapid for a few months after surgery, but it can slow down or stop after a period of time.
A person may not see their desired weight loss until a year or longer after surgery. However, research shows people have an overall sense of improved wellbeing and quality of life after having bariatric surgery.
When is bariatric surgery recommended?
Bariatric surgery may be recommended when diet and exercise changes are not effective.
The American Society for Metabolic and Bariatric Surgery (ASMBS) is the largest professional group of bariatric surgeons in the United States. The ASMBS has endorsed several types of surgeries for weight loss, but their recommendations vary depending on a person’s BMI. In general, the ASMBS recommends bariatric surgery only for:
- People with a BMI of 35 or more
- People with a BMI of 30 or more who also have certain obesity-related conditions, such as diabetes.
If you’re thinking about getting weight loss surgery, the first step is to talk to your doctor about the benefits and risks, and which procedure might be best for you.
Planning for surgery
Planning for bariatric surgery usually takes several months after the initial consult with a bariatric team. This team consists of doctors, nurses, case managers, pharmacists, dietitians, social workers, and psychologists, who work directly with the person throughout their weight loss journey.
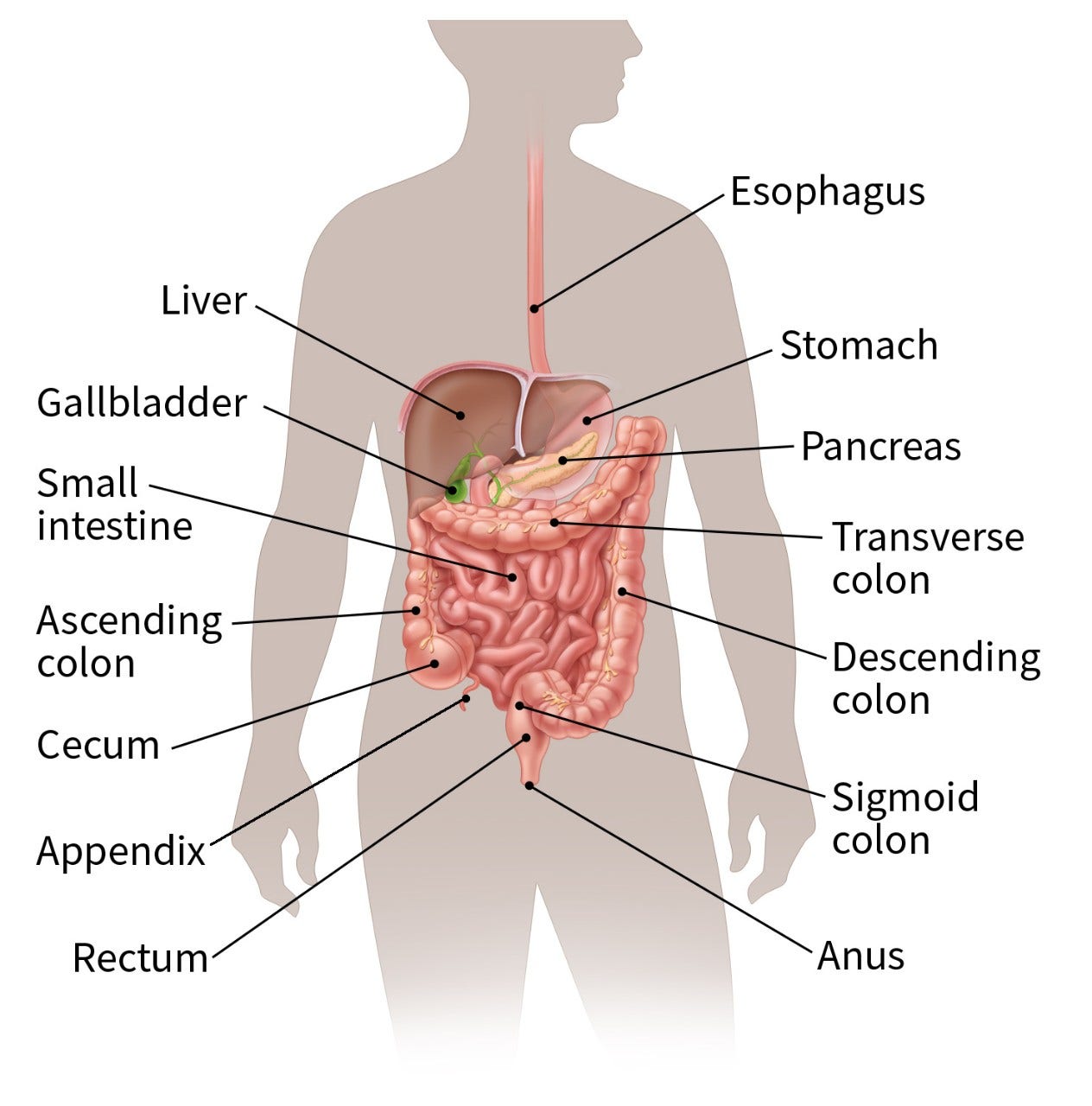
As you learn about the procedures, it may help to look at anatomy images along with a 3D tour of the digestive system to help you see and understand the different parts of the digestive system, also called the gastrointestinal (GI) system.
What are the different types of bariatric surgery?
There are several types of bariatric surgery. Each uses a different method to help with weight loss and improve health. The right option depends on a person’s overall health, weight loss goals, and preferences.
This is the most common type of bariatric surgery in the US. The procedure removes most of the stomach and leaves a small, banana-size shape to the stomach. The “new” stomach is much smaller and holds much less food and fluids. This limits how much the person can eat in one sitting after the surgery. It also helps decrease feelings of being hungry because the stomach size is smaller.
Effect:
- Expected weight loss of about 25% of body weight at 12 months after surgery
Benefits:
- Procedure takes a short time and is simpler than others.
- Weight loss is usually sustained at 5 years.
Risks:
- The procedure cannot be reversed.
- It may trigger new problems like heartburn or gastric reflux. It can also make these problems worse if you already have them.
This procedure involves dividing the stomach into two parts – the upper part becomes a small pouch, and the lower part becomes a larger pouch. The small intestine is also divided, creating a new branch that connects to the smaller upper stomach pouch. The start of the resulting small intestine is in the shape of a Y, with connections to each pouch.
After the procedure, when food is swallowed it goes into the small pouch, then directly into the new branch of the small intestine. Food will bypass the large lower stomach pouch, as well as the first part of the small intestine that’s still connected to it. This limits how much the person can eat in one sitting after the surgery, as well as how much is absorbed by the small intestine. It also helps decrease feelings of being hungry.
Effect:
- Expected weight loss of about 25% of body weight at 12 months after surgery
Benefits:
- Weight loss is usually sustained at 5 years.
- Procedure is reversible.
In this procedure, a silicone band is placed around the upper part of your stomach, creating a small pouch above the band. The band can be adjusted (using a syringe to add or remove fluid from the band) or removed. It may need a few adjustments during the first year. This procedure is less common than gastric sleeve or gastric bypass procedures.
Effect:
- Expected weight loss is less than gastric sleeve or Roux-en-Y gastric bypass.
Benefits:
- The band can be adjusted and is removable.
- There’s less chance of problems right after surgery.
- There’s less risk that vitamins and minerals won’t be absorbed properly compared to gastric bypass surgery.
Risks:
- The band may move and need to be adjusted.
- Sometimes the band can damage the wall of the stomach.
- Some people might have swallowing problems, and their esophagus or the upper stomach pouch may enlarge.
- There is a chance people may not tolerate the band.
Biliopancreatic diversion with duodenal switch (BPD-DS) and single anastomosis duodeno-ileal bypass with sleeve gastrectomy (SADI-S) are newer procedures that are not performed as often in the US. They are typically more complex and can have a higher risk of serious complications.
Can bariatric surgery affect cancer risk?
Bariatric surgery and cancer risk continue to be studied by researchers. Studies on bariatric surgery and cancer risk have had mixed findings.
- Some studies have suggested that bariatric surgery can help lower a person’s risk of breast, endometrial (uterus), colorectal, liver, pancreatic, gallbladder, and ovarian cancers, as well as multiple myeloma. Bariatric surgery has not been found to lower the risk of gastric (stomach), esophageal, prostate, thyroid, or kidney cancer. A few studies have suggested that it might increase the risk of some cancers.
- In people who have cancer, bariatric surgery has been linked with a lower risk of developing a second cancer and dying from cancer.
Talk to your primary care team or cancer care team about options that are best for you.
- Written by
- References

The American Cancer Society medical and editorial content team
Our team is made up of doctors and oncology certified nurses with deep knowledge of cancer care as well as editors and translators with extensive experience in medical writing.
Angrisani L, Santonicola A, Iovino P, et al. IFSO Worldwide Survey 2016: primary, endoluminal, and revisional procedures. Obesity Surgery. 2018;28(12):3783–3794. doi: 10.1007/s11695-018-3450-2.
Caruso A, Gelsomino L, Panza S, et al. Leptin: A heavyweight player in obesity-related cancers. Biomolecules. 2023;13(7):1084.
Eisenberg D, Shikora SA, Aarts E, et al. 2022 American Society for Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO): Indications for Metabolic and Bariatric Surgery. Surg Obes Relat Dis. 2022 Dec;18(12):1345-1356.
Elmaleh-Sachs A, Schwartz JL, Bramante CT, et al. Obesity management in adults: A review. JAMA. 2023 Nov 28;330(20):2000-15. doi:10.1001/jama.2023.1989.
Ganipisetti VM, Bollimunta P. Obesity and set-point theory. [Updated 2023 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Accessed at https://www.ncbi.nlm.nih.gov/books/NBK592402/ on July 30, 2025.
Lim RB. Bariatric procedures for the management of severe obesity: Descriptions. UpToDate. 2023. Accessed at https://www.uptodate.com/contents/bariatric-procedures-for-the-management-of-severe-obesity-descriptions on July 30, 2025.
Lin C, et al. Comparative risk of obesity-related cancer with glucagon-like protein-1 receptor agonists vs. bariatric surgery in patients with BMI >35. Journal of Clinical Oncology. 2024; 42(16):suppl. doi.org/10.1200/JCO.2024.42.16_suppl.10508.
López M, Nogueiras R. Ghrelin. Current Biology. 2023;33(21):R1133-1135. DOI: 10.1016/j.cub.2023.09.009
Wilson RB, Lathigara D, Kaushal D. Systematic review and meta-analysis of the impact of bariatric surgery on future cancer risk. Int J Mol Sci. 2023; 24(7):6192. https://doi.org/10.3390/ijms24076192
Last Revised: September 9, 2025
American Cancer Society medical information is copyrighted material. For reprint requests, please see our Content Usage Policy.
More Resources
More Interactive Tools
American Cancer Society Emails
Sign up to stay up-to-date with news, valuable information, and ways to get involved with the American Cancer Society.







